Adenocarcinoma of the Eye: A Comprehensive Guide
Introduction
Adenocarcinoma is a type of cancer originating in the glandular tissues, which are cells that produce and secrete substances such as mucus, digestive juices, or other fluids. When adenocarcinoma affects the eye, it can involve various ocular and periocular structures, leading to a range of symptoms and necessitating specialized treatment. This article provides an in-depth look at adenocarcinoma of the eye, covering its types, symptoms, diagnosis, treatment options, prognosis, and additional considerations.
Types of Adenocarcinoma in the Eye
Adenocarcinoma can affect different parts of the eye and its associated structures. The main types include:
- Lacrimal Gland Adenocarcinoma
- The lacrimal gland, located in the upper outer region of each orbit (eye socket), is responsible for producing tears. Adenocarcinoma in this gland is rare but aggressive, often leading to significant morbidity.
- Symptoms: Patients typically present with a painless, progressive swelling in the upper eyelid, sometimes accompanied by pain, a feeling of pressure in the orbit, or diplopia (double vision).
- Diagnosis: MRI and CT scans are often used to visualize the mass. A biopsy is required for definitive diagnosis. Additional tests may include blood work to assess overall health and specific markers.
- Treatment: Treatment usually involves surgery to remove the tumor, followed by radiation therapy. In some cases, chemotherapy might be considered if the cancer has spread or if the tumor cannot be completely removed surgically.
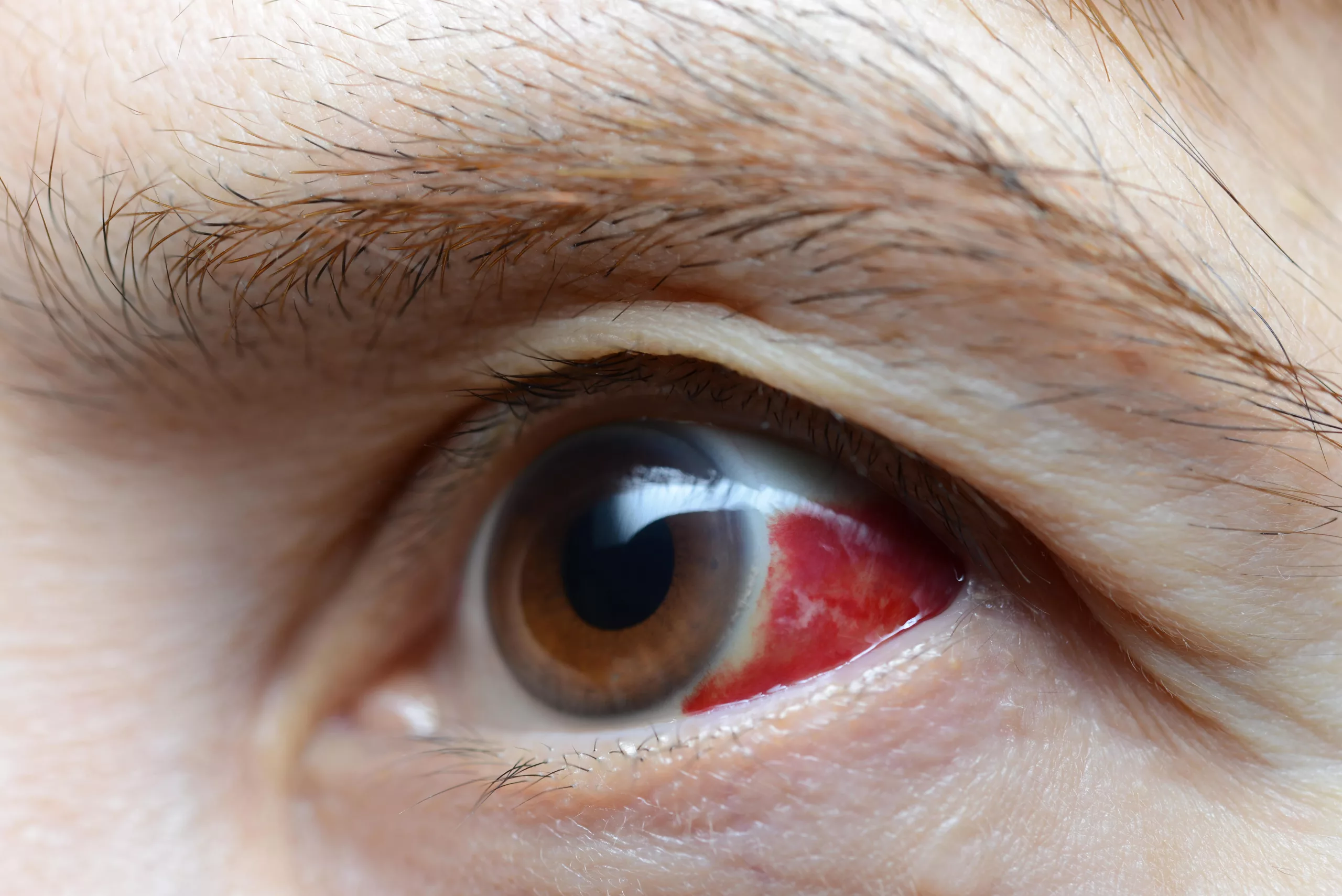
- Conjunctival Adenocarcinoma
- The conjunctiva is a thin, transparent tissue covering the white part of the eye and the inner surface of the eyelids. Adenocarcinoma in this area is also uncommon but can be locally invasive.
- Symptoms: Symptoms include redness, irritation, a visible growth or lesion on the eye surface, and potential vision changes if the lesion interferes with the cornea. Patients might also experience tearing, discharge, or a sensation of a foreign body in the eye.
- Diagnosis: Slit-lamp examination, biopsy, and histopathological analysis are key to diagnosing conjunctival adenocarcinoma. Additional diagnostic tools may include ocular surface cytology and imaging studies to rule out deeper invasion.
- Treatment: Surgical excision of the tumor is the primary treatment. Adjunctive therapies such as cryotherapy (freezing of the tissue), topical chemotherapy, or radiation may be used to reduce recurrence and treat any residual disease.
- Meibomian Gland Adenocarcinoma
- Meibomian glands are located in the tarsal plates of the eyelids and secrete oils that help maintain the tear film. Adenocarcinoma of these glands, also known as sebaceous carcinoma, can mimic benign conditions like chalazia or blepharitis, making early diagnosis challenging.
- Symptoms: Patients may notice a persistent lump in the eyelid, often mistaken for a benign chalazion, eyelid thickening, ulceration, or distortion of the eyelid margin. There may also be associated inflammation or spread to regional lymph nodes.
- Diagnosis: Biopsy and histopathological examination are crucial. Imaging studies like MRI or CT may be used to assess the extent of the disease. Sentinel lymph node biopsy can help determine the spread of the cancer.
- Treatment: Treatment involves wide surgical excision with clear margins. Sentinel lymph node biopsy and adjuvant radiation therapy might be necessary if there is a high risk of metastasis. Reconstructive surgery may be required following extensive excisions.
Symptoms
The symptoms of adenocarcinoma of the eye vary depending on the affected area but generally include:
- Lacrimal Gland Adenocarcinoma: Swelling, pain, diplopia (double vision), and a noticeable mass in the upper outer region of the eye socket. Patients may also experience restricted eye movement and proptosis (bulging of the eye).
- Conjunctival Adenocarcinoma: Redness, irritation, a visible growth on the eye surface, and potential vision changes. Additional symptoms can include tearing, discharge, and a sensation of a foreign body in the eye.
- Meibomian Gland Adenocarcinoma: Swelling of the eyelid, a persistent lump, potential eyelid deformity, ulceration, and thickening. There may be associated inflammation and spread to nearby lymph nodes.
- Additional Symptoms Across Types: Blurred vision, decreased eye movement, discomfort or pain in and around the eye, and sometimes systemic symptoms if the cancer has metastasized.
Diagnosis
Diagnosing adenocarcinoma of the eye involves several steps:
- Clinical Examination:
- A thorough clinical examination by an ophthalmologist or ocular oncologist is the first step. This includes:
- Visual Acuity Test: To assess any impact on vision.
- Slit-Lamp Examination: To examine the eye under high magnification and identify any abnormalities on the eye surface or within the eye.
- Palpation: To feel for any masses or abnormalities in the eye or orbit.
- Fundoscopy: Examination of the retina and optic nerve to check for any changes or signs of metastasis.
- Imaging Studies:
- Imaging techniques help determine the size, location, and extent of the tumor. Common imaging studies include:
- MRI (Magnetic Resonance Imaging): Provides detailed images of the eye’s soft tissues and can help distinguish between different tissue types.
- CT (Computed Tomography) Scan: Offers detailed cross-sectional images, particularly useful for evaluating bony structures and tumor extent. It can also detect any calcification within the tumor.
- Ultrasound: Often used to assess intraocular tumors and provide information on their size and internal characteristics.
- PET (Positron Emission Tomography) Scan: May be used in advanced cases to detect metastasis by highlighting areas of increased metabolic activity.
- Biopsy:
- A biopsy involves taking a small tissue sample from the tumor. Techniques include:
- Incisional Biopsy: Removing a part of the tumor, often used when the tumor is large or in a difficult location.
- Excisional Biopsy: Removing the entire tumor, typically used for smaller lesions.
- Fine Needle Aspiration (FNA): Using a thin needle to extract cells for examination, often guided by ultrasound or CT imaging.
- Sentinel Lymph Node Biopsy: To check for the spread of cancer to nearby lymph nodes, particularly in cases of meibomian gland adenocarcinoma.
- Histopathological Analysis: The tissue sample is examined under a microscope by a pathologist to confirm the diagnosis and determine the cancer type and grade. Immunohistochemical staining and molecular testing may be used to identify specific markers and characteristics of the tumor.
- Genetic and Molecular Testing: In some cases, genetic and molecular testing may be performed to identify specific mutations or markers that can guide targeted therapy. These tests can provide information on the prognosis and potential response to certain treatments.
Treatment
The treatment for adenocarcinoma of the eye depends on the tumor’s location, size, and stage. Common treatment options include:
- Surgery:
- Surgical removal of the tumor is often the primary treatment. The extent of surgery depends on the tumor’s location and size:
-
- Local Excision: Removing the tumor with a margin of healthy tissue, typically used for smaller, well-defined tumors.
- Orbitotomy: A surgical procedure to access tumors within the orbit. This may involve removing part of the orbital bone to reach the tumor.
- Enucleation: Removal of the entire eye, typically considered in advanced cases where the tumor cannot be otherwise controlled or if it poses a significant risk to the patient’s health.
- Exenteration: Removal of the eye and surrounding tissues, including the eyelids and orbital contents, used in extensive disease where there is significant local invasion.
- Radiation Therapy:
- Radiation therapy uses high-energy rays to target and kill cancer cells. Types of radiation therapy include:
- External Beam Radiation Therapy (EBRT): Directs radiation at the tumor from outside the body. Techniques such as intensity-modulated radiation therapy (IMRT) can deliver precise doses to minimize damage to surrounding tissues.
- Brachytherapy: Involves placing radioactive material close to or inside the tumor. This technique is often used for localized tumors and can deliver high doses of radiation directly to the tumor while sparing surrounding tissues.
- Chemotherapy:
- Chemotherapy involves using drugs to kill cancer cells. It can be administered systemically (throughout the body) or locally (directly to the tumor site). Chemotherapy is often used for:
- Systemic Disease: When the cancer has spread beyond the eye.
- Adjuvant Therapy: After surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
- Neoadjuvant Therapy: Before surgery to shrink the tumor and make it more manageable for removal.
- Targeted Therapy:
- Targeted therapy uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Examples include:
- Monoclonal Antibodies: Designed to target specific proteins on cancer cells. For example, bevacizumab targets vascular endothelial growth factor (VEGF) to inhibit tumor angiogenesis.
- Small Molecule Inhibitors: Target specific pathways or mutations within cancer cells. For instance, tyrosine kinase inhibitors can block signals that promote cancer cell growth.
- Immunotherapy:
- Immunotherapy boosts the body’s immune system to fight cancer. Types of immunotherapy include:
- Checkpoint Inhibitors: Drugs that block proteins used by cancer cells to avoid detection by the immune system. For example, pembrolizumab targets the PD-1/PD-L1 pathway.
- Adoptive Cell Transfer: Involves collecting and using a patient’s immune cells to attack cancer cells. CAR-T cell therapy is a type of adoptive cell transfer where T cells are modified to better recognize and kill cancer cells.
- Cryotherapy: Cryotherapy involves freezing the tumor cells using liquid nitrogen or argon gas. This treatment is typically used for small, localized tumors and can be combined with other therapies to enhance effectiveness.
- Photodynamic Therapy (PDT): PDT uses light-sensitive drugs and a specific type of light to kill cancer cells. The drug is administered intravenously and accumulates in the tumor cells. When exposed to light of a specific wavelength, the drug activates and destroys the cancer cells.
- Clinical Trials: Patients may have the option to participate in clinical trials, which offer access to new and experimental treatments. These trials can provide additional treatment options and contribute to advancing medical knowledge.
Prognosis
The prognosis for adenocarcinoma of the eye varies based on several factors:
- Tumor Location and Size
-
- Lacrimal Gland Adenocarcinoma: Generally has a poor prognosis due to its aggressive nature and potential for local invasion and metastasis. Early detection and treatment are crucial for improving outcomes.
- Conjunctival Adenocarcinoma: The prognosis is relatively better if detected early and treated promptly. Recurrence and local spread can affect outcomes.
- Meibomian Gland Adenocarcinoma: The prognosis depends on the stage at diagnosis and the extent of local and regional spread. Early-stage tumors have a better prognosis, while advanced disease can be challenging to treat.
- Tumor Stage
-
- Early-Stage Disease: Tumors confined to the primary site without regional or distant spread have a better prognosis and are more amenable to curative treatment.
- Advanced-Stage Disease: Tumors that have spread to nearby tissues, lymph nodes, or distant organs have a poorer prognosis and often require more aggressive treatment.
- Treatment Response
-
- Complete Response: Achieving complete removal or destruction of the tumor is associated with a better prognosis.
- Partial Response: Partial reduction in tumor size may require additional treatments and is associated with a variable prognosis.
- Patient’s Overall Health
-
- Comorbidities: Patients with other health conditions may have a more challenging time tolerating aggressive treatments.
- Age: Younger patients generally have a better prognosis, although this is not always the case.
- Genetic and Molecular Factors
-
- Tumor Genetics: Certain genetic mutations and molecular characteristics can influence prognosis and guide targeted therapies.
- Recurrence
-
- Local Recurrence: Recurrence of the tumor in the same area can complicate treatment and affect prognosis.
- Metastasis: Spread of the tumor to distant sites significantly worsens the prognosis.
Survival Rates
Survival rates depend on the specific type of adenocarcinoma and its stage at diagnosis. Early-stage cancers generally have better outcomes, while advanced stages with metastasis have poorer prognoses.
Follow-Up Care
Regular follow-up is essential for managing adenocarcinoma of the eye. This involves:
- Regular Eye Exams
-
- Frequency: Typically every 3-6 months initially, then annually after several years of stability.
- Components: Visual acuity tests, slit-lamp examinations, and fundoscopy to monitor for recurrence or new issues.
- Imaging Studies
-
- MRI and CT Scans: To monitor for recurrence or metastasis.
- Ultrasound: For assessing intraocular structures.
- Biopsy
- Repeat Biopsy: May be necessary if there are signs of recurrence or new suspicious lesions.
- Blood Tests
- Tumor Markers: Monitoring specific markers in the blood can help detect recurrence early.
- Multidisciplinary Care
- Ophthalmologists: For ongoing eye care and monitoring.
- Oncologists: For systemic management and treatment of any metastases.
- Radiologists: For imaging and interpretation of scans.
Managing Side Effects
Patients undergoing treatment for adenocarcinoma of the eye may experience side effects. Managing these involves a multidisciplinary approach:
- Medical Management
-
- Medications: To control pain, inflammation, and other symptoms.
- Nutritional Support: Ensuring proper nutrition to support recovery and overall health.
- Physical Therapy
-
- Rehabilitation: To help patients regain strength and function, particularly if they have undergone extensive surgery or radiation.
- Psychological Support
-
- Counseling: To address the emotional impact of cancer and its treatment.
- Lifestyle Modifications
-
- Healthy Diet: To support overall health and recovery.
- Exercise: To maintain physical fitness and well-being.
Conclusion
Adenocarcinoma of the eye, though rare, presents significant challenges due to its aggressive nature and potential impact on ocular health and vision. Early detection, accurate diagnosis, and appropriate treatment are crucial for improving outcomes. Through comprehensive education and support, patients and their families can navigate this complex condition with greater confidence and hope for the future.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Early signs include painless swelling, redness, irritation, or a visible growth on the eye surface. Some patients may also experience blurred vision or a sensation of a foreign body in the eye.
Adenocarcinoma of the eye is very rare compared to other types of eye cancers. It represents a small fraction of all ocular tumors.
Yes, like other cancers, adenocarcinoma of the eye can metastasize to other parts of the body, including regional lymph nodes, liver, lungs, and bones.
Adenocarcinoma of the eye can occur at any age, but it is more commonly diagnosed in adults, particularly those over the age of 50.
Known risk factors include a history of radiation exposure, certain genetic conditions, chronic inflammation or irritation, and previous cancers.
You should see an ophthalmologist, specifically one who specializes in ocular oncology. They have the expertise to diagnose and treat eye cancers.
While most cases are sporadic, there can be a genetic predisposition, especially in individuals with certain hereditary cancer syndromes.
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, avoiding tobacco, and managing stress, can support overall health and recovery during treatment.
Quality of life can be affected by treatment, particularly if it involves extensive surgery or radiation. Patients may need to adapt to changes in vision and appearance, and psychological support can be beneficial.
Advances include targeted therapies, immunotherapies, and improved surgical techniques that enhance treatment effectiveness and reduce side effects. Ongoing research continues to explore new treatment options.
news via inbox
Subscribe here to get latest updates !