Corneal Ulcers: Causes, Symptoms, and Timely Treatment
Corneal ulcers are serious eye infections that can lead to vision impairment if not promptly addressed. This article provides a comprehensive overview of the symptoms, causes, risk factors, diagnosis, treatment, and prevention of corneal ulcers. It offers valuable insights for individuals experiencing eye discomfort and those seeking information on maintaining corneal health.
Overview of Corneal Ulcers
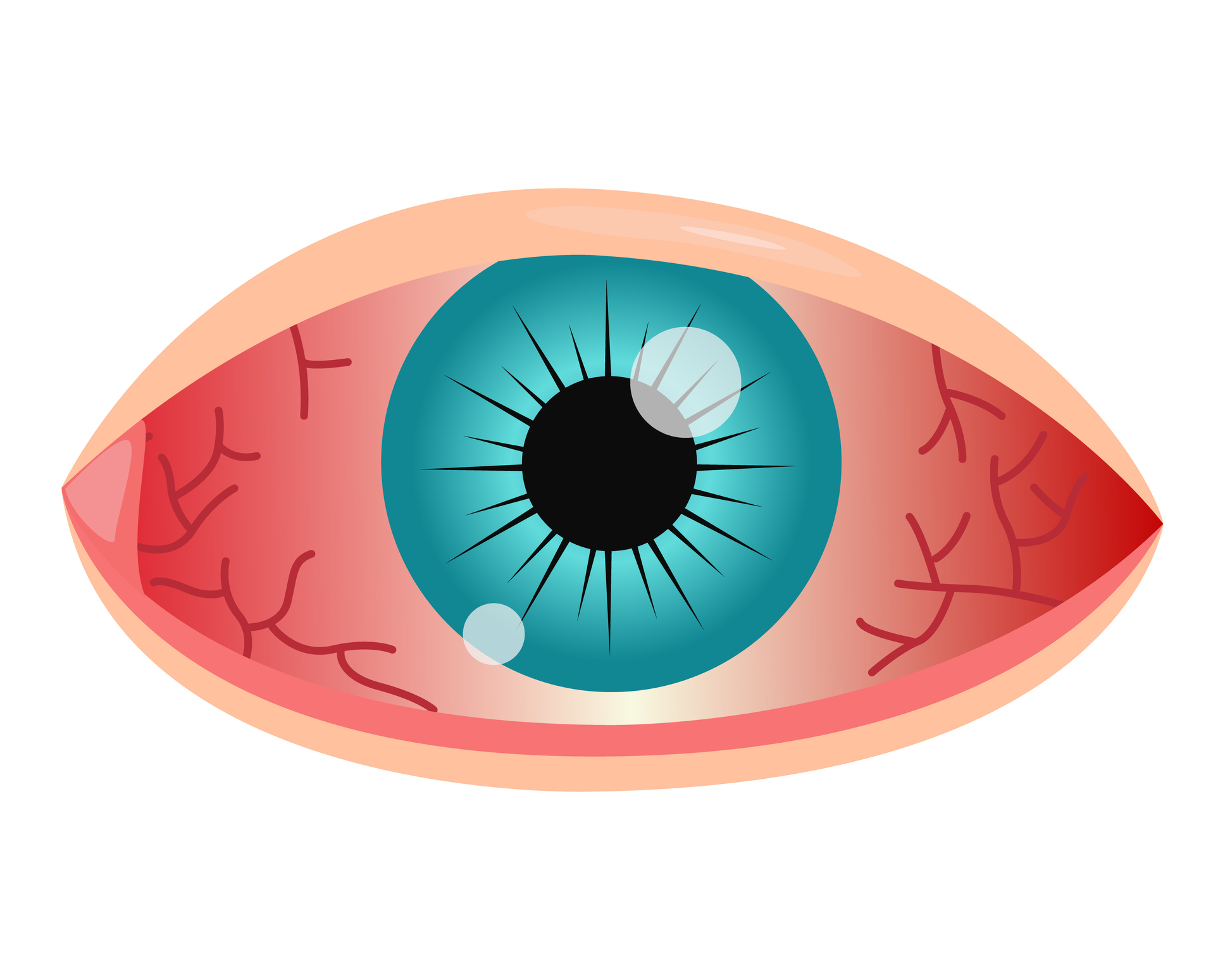
The cornea is the transparent, dome-shaped front part of the eye that covers the iris and pupil. Corneal ulcers are open sores on the cornea, often caused by infections, trauma, or underlying conditions. These ulcers can range in size and depth, and their severity can vary. They are a serious condition that requires prompt attention to prevent complications.
Symptoms
- Eye Pain: Corneal ulcers typically cause significant pain, often described as a sharp, stabbing sensation.
- Redness: The affected eye appears red due to inflammation and increased blood flow to the area.
- Tearing: Excessive tearing or watery eyes are common as the eye responds to the irritation.
- Sensitivity to Light: Photophobia, or heightened sensitivity to light, is a typical symptom and can worsen the discomfort.
Causes
- Bacterial Infections: Common bacteria like Staphylococcus or Pseudomonas can invade the cornea, leading to ulcers.
- Viral Infections: Herpes simplex virus (HSV) or varicella-zoster virus (VZV) can cause viral keratitis and corneal ulcers.
- Fungal Infections: Fungi such as Candida or Fusarium can lead to corneal ulcers, particularly in individuals with compromised immune systems.
- Trauma: Injuries to the cornea, such as scratches from foreign bodies or contact lenses, can result in ulcers.
- Contact Lens Use: Improper use, hygiene, or extended wear of contact lenses can introduce pathogens, increasing the risk.
What Happens Because of the Condition
- Corneal Damage: Ulcers damage the corneal tissue, affecting its transparency and structural integrity.
- Inflammation: Inflammatory responses, including redness and swelling, are common as the body tries to fight the infection.
- Vision Impairment: Depending on the size and location of the ulcer, visual acuity may be affected, leading to blurred or distorted vision.
Risk Factors
- Contact Lens Wear: Extended use, poor hygiene, or using contact lenses in environments like swimming pools can increase the risk.
- Eye Trauma: Scratches, foreign objects, or injuries to the eye can make it more susceptible to infections and ulcers.
- Reduced Immune Function: Conditions or medications that weaken the immune system make individuals more vulnerable to infections leading to ulcers.
- Dry Eye Syndrome: Inadequate tear production or poor tear quality can compromise the cornea’s defense mechanisms.
- Underlying Eye Conditions: Conditions like blepharitis (inflammation of the eyelids), keratitis (inflammation of the cornea), or previous eye surgeries may predispose individuals to corneal ulcers.
Understanding these factors is crucial for both prevention and early intervention. If someone experiences symptoms indicative of a corneal ulcer, seeking immediate medical attention from an eye care professional is imperative. Timely diagnosis and appropriate treatment can prevent complications and help preserve vision.
Diagnosis
- Clinical Examination: An eye care professional will conduct a thorough examination, evaluating symptoms, visual acuity, and the appearance of the cornea.
- Slit Lamp Exam: A slit lamp is used to magnify and illuminate the cornea, aiding in a detailed assessment.
- Corneal Staining: Fluorescein or rose bengal dye may be used to highlight corneal defects for better visualization.
- Cultures and Smears: Collecting samples for microbial cultures or smears helps identify the causative agent, informing targeted treatment.
- Visual Acuity Test: Assessing the clarity of vision to determine the extent of visual impairment.
Treatment Options
- Topical Antibiotics: Broad-spectrum antibiotics, such as fluoroquinolones, are commonly prescribed to combat bacterial infections.
- Antiviral Medications: For viral infections, antiviral medications like acyclovir may be used.
- Antifungal Medications: Fungal infections may require antifungal medications, either topical or systemic.
- Corticosteroids: In some cases, corticosteroid eye drops are used cautiously to reduce inflammation, but their use depends on the underlying cause.
- Pain Management: Analgesics or topical anesthetics may be prescribed to alleviate pain and discomfort.
Complications
- Scarring: Severe ulcers may lead to corneal scarring, impacting vision.
- Corneal Perforation: In extreme cases, persistent ulcers can lead to a hole in the cornea, requiring urgent intervention.
- Vision Loss: Untreated or inadequately managed corneal ulcers can result in permanent vision impairment or blindness.
Prevention
- Hygiene Practices: Proper handwashing and contact lens care, including regular cleaning and disinfection, reduce the risk.
- Protective Eyewear: Wearing protective eyewear in situations prone to eye injuries can prevent trauma.
- Regular Eye Exams: Routine eye examinations can help identify and address risk factors early on.
- Immediate Treatment of Injuries: Seek prompt medical attention for any eye injuries to prevent infection and complications.
Medications
- Topical Antibiotics: Examples include ciprofloxacin or moxifloxacin for bacterial infections.
- Antiviral Medications: Acyclovir or ganciclovir may be prescribed for viral infections.
- Antifungal Medications: Agents like amphotericin B or voriconazole for fungal ulcers.
- Corticosteroids: Prednisolone or dexamethasone eye drops may be used cautiously in certain cases.
When to See a Doctor
- Sudden Eye Pain: Immediate medical attention is warranted for sudden and severe eye pain.
- Visual Changes: Any sudden changes in vision, especially if accompanied by pain, require prompt evaluation.
- Contact Lens-related Issues: If using contact lenses and experiencing discomfort or redness, consult a doctor.
Demographics More Susceptible
- Contact Lens Wearers: Especially those who do not adhere to proper hygiene practices.
- People with Compromised Immune Systems: Conditions like HIV/AIDS or those on immunosuppressive medications.
- Elderly Individuals: Age-related changes may increase susceptibility to corneal ulcers.
Follow-up Care for Adults and Children
For Adults:
- Medication Adherence: Strict adherence to prescribed medications, especially antibiotics.
- Regular Eye Exams: Routine follow-ups to monitor healing and address any complications.
For Children:
- Parental Guidance: Ensuring children adhere to prescribed treatments.
- Educational Support: Providing resources and support for any visual or developmental challenges.
Conclusion
In conclusion, corneal ulcers demand swift and accurate diagnosis, followed by targeted treatment to prevent complications and preserve vision. Individuals should prioritize eye hygiene, seek prompt medical attention for injuries, and adhere to prescribed treatments. Regular eye examinations are key for early detection and prevention of corneal ulcers. Collaborative efforts between healthcare providers and individuals are vital for successful management and optimal outcomes.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Corneal Ulcers, if not treated promptly, can lead to permanent vision damage. Seeking professional advice and adhering to prescribed care plans are crucial for preserving vision.
Over-the-counter eye drops are not sufficient for treating Corneal Ulcers. Professional evaluation and prescription medications are necessary for effective management.
Proper eye hygiene, avoiding eye injuries, and following contact lens care guidelines are essential for preventing Corneal Ulcers. Seeking prompt care for eye issues is also crucial.
While allergies can cause eye irritation, Corneal Ulcers are more commonly associated with infections or injuries. Allergy management may be part of the overall care plan.
Recurrence of Corneal Ulcers is possible, especially if the underlying cause is not fully addressed. Regular follow-up appointments and ongoing care may be necessary.
Surgery may be necessary in severe cases or if complications arise. However, many Corneal Ulcers can be effectively managed with medications and non-surgical interventions.
Corneal Ulcers are often associated with eye pain, redness, and discomfort. Pain management may be part of the overall care plan.
Yes, viral infections, such as herpes simplex virus, can cause Corneal Ulcers. Prompt antiviral treatment is essential in such cases.
Vision loss can occur if Corneal Ulcers are left untreated or if complications arise. Early diagnosis and appropriate care are crucial for preventing vision impairment.
Yes, contact lens wearers are at a higher risk of Corneal Ulcers, especially if proper hygiene practices are not followed. Regular eye check-ups and adherence to lens care guidelines are essential.
news via inbox
Subscribe here to get latest updates !