Delving Deeper into Lacrimal Gland Prolapse
Introduction
Lacrimal gland prolapse is a condition that demands meticulous attention and understanding due to its potential impact on ocular health and overall well-being. In this extensive examination, we unravel the intricacies of lacrimal gland prolapse, encompassing its etiology, clinical manifestations, diagnostic intricacies, treatment modalities, and broader implications for ocular health.
Etiological Insights into Lacrimal Gland Prolapse
Lacrimal gland prolapse can arise from a myriad of factors, each contributing to the disruption of the gland’s normal anatomical position within the orbit:
- Traumatic Events: Direct trauma to the orbital region, whether from accidents, falls, or blunt force trauma, can precipitate the displacement of the lacrimal gland. Such trauma may compromise the integrity of the gland’s surrounding supportive structures, leading to prolapse.
- Anatomical Variations: Anatomical anomalies within the orbit, both congenital and acquired, can predispose individuals to lacrimal gland prolapse. These variations may include orbital asymmetry, bony prominences, or defects in the orbital septum, altering the spatial relationship between the lacrimal gland and its surrounding structures.
- Underlying Conditions: Systemic disorders such as thyroid eye disease, orbital tumors, or inflammatory conditions like Graves’ disease or sarcoidosis, may indirectly contribute to lacrimal gland prolapse. These conditions can exert pressure on the orbital contents, disrupting the equilibrium within the orbit and facilitating gland displacement.
Exploring the Clinical Spectrum
The clinical manifestations of lacrimal gland prolapse encompass a broad spectrum of symptoms and signs, each offering valuable insights into the condition’s severity and impact:
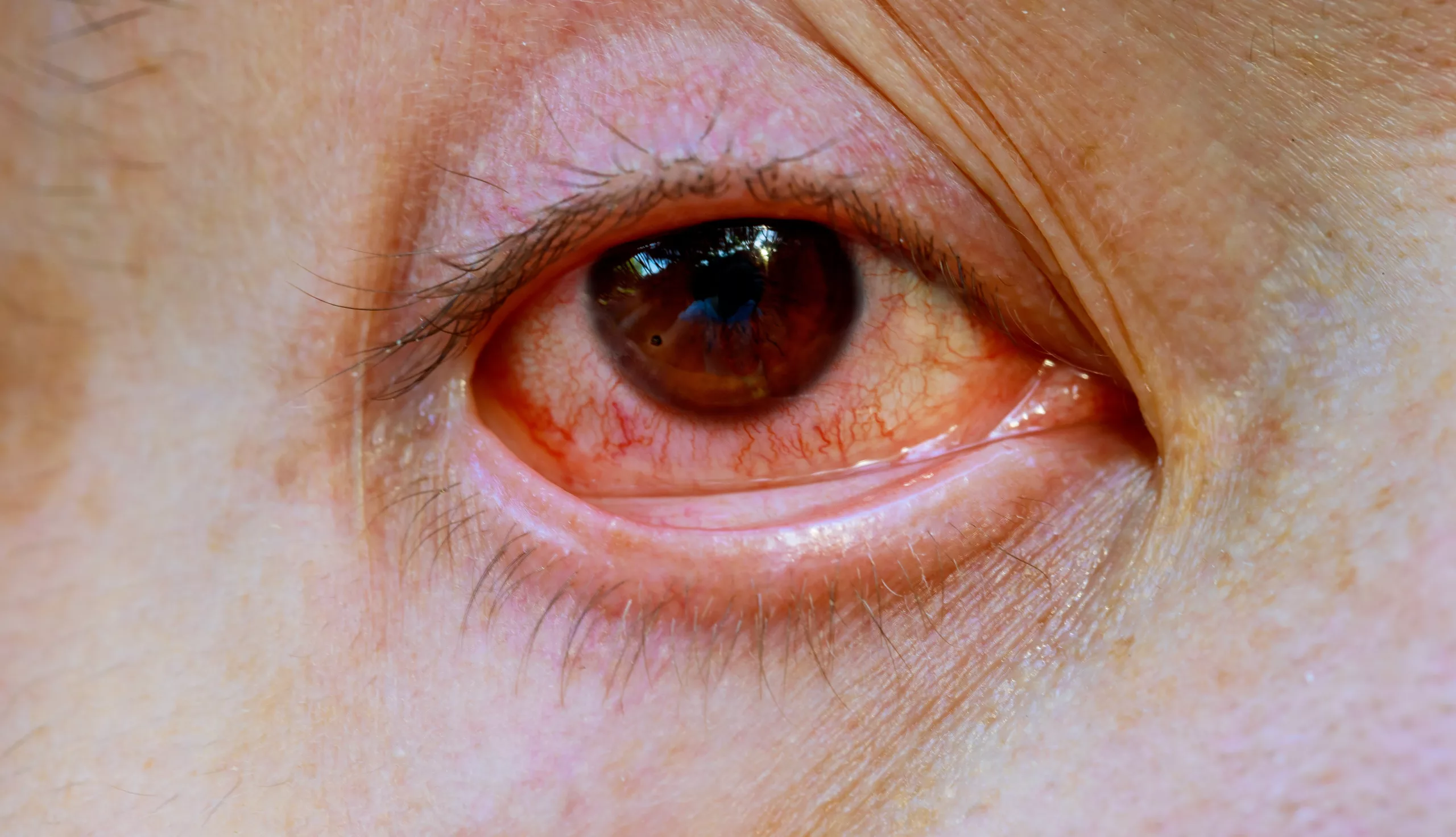
- Visible Swelling: A palpable or visible protrusion of the lacrimal gland beneath the eyelid or within the orbit is the hallmark feature of lacrimal gland prolapse. The gland may appear as a rounded or elongated mass, often accompanied by erythema or edema of the surrounding tissues.
- Ocular Discomfort: Patients frequently report sensations of pressure, heaviness, or discomfort around the affected eye. These symptoms may be exacerbated by blinking, eye movements, or prolonged periods of visual tasks, reflecting the mechanical irritation caused by the displaced gland.
- Visual Disturbances: In advanced cases, lacrimal gland prolapse may encroach upon the visual axis, leading to visual disturbances such as blurriness, double vision, or visual field deficits. These symptoms underscore the potential impact of gland displacement on ocular function and visual acuity.
Navigating the Diagnostic Labyrinth
Accurate diagnosis of lacrimal gland prolapse hinges on a systematic approach, integrating clinical examination findings with supplemental diagnostic modalities:
- Clinical Examination: A comprehensive evaluation of the eyelids, orbit, and ocular surface is paramount for identifying signs of lacrimal gland prolapse. Palpation of the orbital rim may reveal a palpable mass corresponding to the displaced gland, while visual inspection can elucidate associated features such as erythema, edema, or conjunctival injection.
- Imaging Studies: Supplemental imaging modalities such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) may be utilized to further characterize the extent and nature of gland displacement. These imaging studies can provide detailed anatomical information, guiding treatment planning and surgical intervention.
Tailoring Therapeutic Strategies
The management of lacrimal gland prolapse is contingent upon individualized factors, including the severity of symptoms, functional impairment, and underlying etiology:
- Conservative Measures: Asymptomatic or minimally symptomatic cases of lacrimal gland prolapse may initially warrant conservative management. This may include symptomatic relief measures such as warm compresses, lubricating eye drops, or topical anti-inflammatory medications to alleviate ocular discomfort and inflammation.
- Surgical Intervention: Symptomatic or refractory cases of lacrimal gland prolapse often necessitate surgical correction to restore the gland to its normal anatomical position within the orbit. Surgical techniques may vary depending on the specific characteristics of the prolapse, the patient’s ocular anatomy, and the surgeon’s expertise. Common surgical approaches include gland repositioning, stabilization, or removal, aiming to alleviate symptoms and prevent recurrence.
Appreciating the Broader Implications
Lacrimal gland prolapse extends beyond its immediate clinical manifestations, exerting broader implications for ocular health and overall quality of life:
- Chronic Discomfort: Untreated or inadequately managed cases of lacrimal gland prolapse can lead to persistent ocular discomfort, compromising patients’ quality of life and visual well-being. Chronic irritation, inflammation, and mechanical pressure on ocular structures may exacerbate symptoms, necessitating prompt intervention to alleviate discomfort and restore ocular comfort.
- Complications: Long-term complications of lacrimal gland prolapse may include corneal exposure, dry eye syndrome, or secondary infections. These complications can further exacerbate ocular discomfort and compromise visual function, underscoring the importance of timely diagnosis and appropriate management to mitigate the risk of complications and optimize treatment outcomes.
Conclusion
In conclusion, lacrimal gland prolapse represents a complex interplay of anatomical, mechanical, and pathological factors, necessitating a multifaceted approach to diagnosis and management. By fostering understanding and awareness of lacrimal gland prolapse’s intricacies, patients and healthcare providers can navigate its challenges effectively, ultimately promoting optimal ocular health and enhancing patients’ overall well-being. Through collaborative care, individualized treatment strategies, and proactive intervention, individuals grappling with lacrimal gland prolapse can embark on a journey toward improved ocular comfort, visual clarity, and quality of life, reclaiming the vitality and resilience of their ocular ecosystem.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
With proper treatment, most individuals can achieve significant relief from symptoms and prevent complications, leading to improved ocular comfort and quality of life.
Maintaining good ocular hygiene, avoiding eye trauma, and managing underlying conditions like thyroid eye disease can help reduce the risk and impact of lacrimal gland prolapse.
Timely diagnosis and appropriate management are crucial. Adhering to prescribed treatments and regular follow-ups can prevent complications like corneal exposure and dry eye syndrome.
Surgical intervention is generally safe and effective, tailored to the patient’s specific anatomy and prolapse characteristics, though it carries standard surgical risks.
Treatment ranges from conservative approaches for mild cases to surgical interventions for symptomatic or severe prolapse, aimed at repositioning or stabilizing the gland.
While minor cases might improve with conservative measures like warm compresses and lubricating eye drops, significant or symptomatic prolapse typically requires medical or surgical intervention.
Diagnosis involves a clinical examination of the eyelids and orbit, supplemented by imaging studies such as ultrasound, CT, or MRI to detail the extent of gland displacement.
Symptoms include visible swelling or a palpable mass beneath the eyelid, ocular discomfort, and potential visual disturbances like blurriness or double vision.
Common causes include traumatic events, anatomical variations within the orbit, and underlying conditions such as thyroid eye disease or orbital tumors that exert pressure on the gland.
Lacrimal gland prolapse occurs when the lacrimal gland, responsible for tear production, displaces from its normal anatomical position, leading to visible swelling and discomfort around the eye.
news via inbox
Subscribe here to get latest updates !