Managing Diabetic Retinopathy Causes, Symptoms
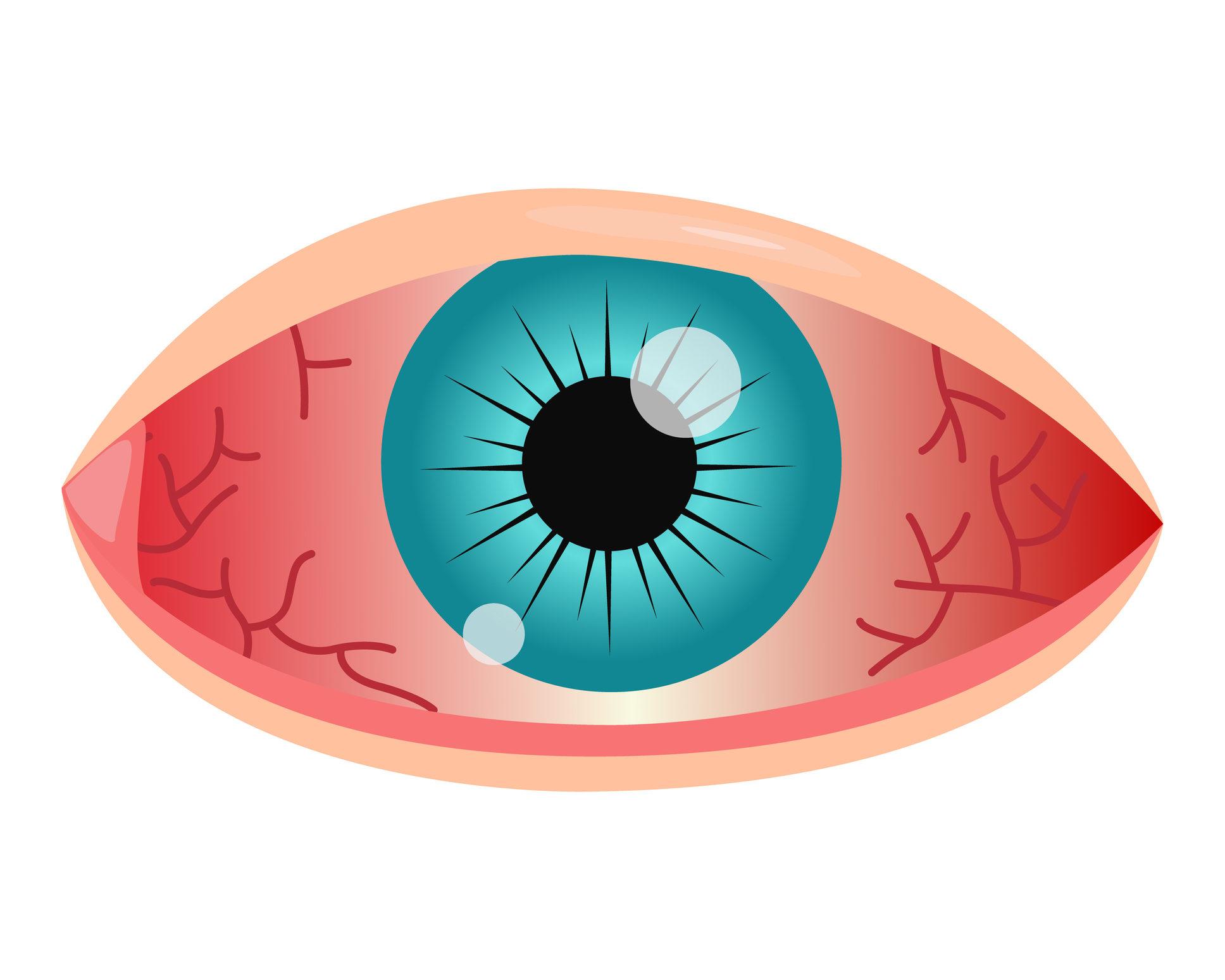
Diabetic Retinopathy is a complication of diabetes that affects the eyes, potentially leading to vision loss. This article provides a comprehensive overview of the symptoms, causes, risk factors, diagnosis, treatment, and prevention of Diabetic Retinopathy, offering essential information for individuals managing diabetes and those seeking to protect their vision.
Overview of Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes that affects the eyes. It results from damage to the blood vessels of the retina, the light-sensitive tissue at the back of the eye. Over time, diabetic retinopathy can lead to vision impairment or blindness if left untreated. It is a significant cause of visual loss among individuals with diabetes.
Symptoms
- Blurred Vision: Blurriness or fluctuations in vision can occur.
- Floaters: The perception of dark spots or floating debris in the field of vision.
- Impaired Color Vision: Difficulty perceiving colors accurately.
- Dark or Empty Areas: The presence of dark or empty areas in the visual field may indicate advanced stages of the condition.
Causes
Diabetic retinopathy is primarily caused by long-term diabetes and its impact on the blood vessels in the retina. The elevated levels of blood sugar associated with diabetes can lead to:
- Microvascular Damage: Damage to the small blood vessels in the retina.
- Ischemia: Reduced blood flow to the retina, triggering the growth of abnormal blood vessels.
- Fluid Leakage: Weakening of blood vessel walls, leading to fluid leakage into the retina.
What Happens Because of the Condition
- Non-Proliferative Diabetic Retinopathy (NPDR): In the early stage, microaneurysms and small bleeding occur in the retina, leading to mild vision changes.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage involving the growth of abnormal blood vessels, which are fragile and prone to bleeding. Scar tissue formation may occur.
- Macular Edema: Fluid accumulation in the macula, the central part of the retina responsible for sharp, central vision, leading to further visual impairment.
Risk Factors
- Duration of Diabetes: The longer an individual has diabetes, the higher the risk of developing diabetic retinopathy.
- Poor Blood Sugar Control: Inadequate management of blood sugar levels increases the risk of vascular damage.
- High Blood Pressure: Hypertension can exacerbate the progression of diabetic retinopathy.
- High Cholesterol Levels: Elevated levels of cholesterol can contribute to the development and progression of the condition.
- Pregnancy: Pregnant individuals with diabetes may be at a higher risk, and diabetic retinopathy can worsen during pregnancy.
Understanding these risk factors is crucial for regular eye screenings, especially for individuals with diabetes, to detect diabetic retinopathy in its early stages when intervention is most effective.
Diagnosis
Diagnosing diabetic retinopathy involves a comprehensive eye examination, which may include:
- Dilated Eye Exam: The eye is dilated with eye drops to allow the eye care professional to examine the retina and optic nerve for signs of diabetic retinopathy.
- Visual Acuity Test: Assessing the clarity of vision to detect any changes.
- Fluorescein Angiography: A dye is injected into the bloodstream, and retinal photographs are taken to identify areas of blood vessel leakage.
- Optical Coherence Tomography (OCT): This imaging test provides detailed cross-sectional images of the retina, helping to detect swelling or fluid accumulation.
Treatment Options
- Optimal Diabetes Management: Strict control of blood sugar levels, blood pressure, and cholesterol is fundamental to slowing the progression of diabetic retinopathy.
- Laser Therapy (Photocoagulation): Laser treatment can seal leaking blood vessels or eliminate abnormal blood vessels to prevent further damage.
- Intravitreal Injections: Medications, such as anti-VEGF drugs, may be injected into the eye to reduce the growth of abnormal blood vessels and manage macular edema.
- Vitrectomy: In advanced cases with significant bleeding into the vitreous, a surgical procedure called vitrectomy may be performed to remove blood and scar tissue.
Complications
- Macular Edema: Swelling in the macula can lead to blurred or distorted central vision.
- Proliferative Diabetic Retinopathy (PDR): Abnormal blood vessels may bleed into the vitreous, causing floaters and potentially leading to retinal detachment.
- Retinal Detachment: The abnormal growth of blood vessels and scar tissue can contribute to the pulling away of the retina from the underlying tissue.
- Glaucoma: Neovascular glaucoma, a form of glaucoma associated with diabetic retinopathy, can lead to increased pressure within the eye.
Prevention
- Regular Eye Examinations: Individuals with diabetes should undergo regular eye screenings, even in the absence of symptoms, to detect diabetic retinopathy in its early stages.
- Blood Sugar Control: Maintaining target blood sugar levels is crucial in preventing and slowing the progression of diabetic retinopathy.
- Blood Pressure and Cholesterol Management: Controlling blood pressure and cholesterol levels reduces the risk of vascular damage in the eyes.
- Lifestyle Modifications: A healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, can contribute to overall eye health.
Medications
- Anti-VEGF Injections: Drugs such as bevacizumab, ranibizumab, and aflibercept may be injected into the eye to inhibit the growth of abnormal blood vessels.
- Corticosteroids: In certain cases, corticosteroids may be used to reduce inflammation and manage macular edema.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to address inflammation.
It’s essential for individuals with diabetic retinopathy to work closely with their healthcare team to determine the most appropriate treatment approach based on the specific characteristics and stage of the condition.
When to See a Doctor
- Diabetes Diagnosis: Individuals diagnosed with diabetes should schedule an eye examination promptly, even if there are no apparent vision problems.
- Regular Eye Exams: For those with diabetes, regular eye examinations are crucial, typically at least once a year. More frequent exams may be recommended if diabetic retinopathy is detected.
- Vision Changes: Any sudden or gradual changes in vision, such as blurriness, floaters, or difficulty seeing clearly, should prompt an immediate visit to an eye care professional.
- Pregnancy: Pregnant individuals with diabetes or gestational diabetes should discuss with their healthcare provider and ophthalmologist for appropriate eye care during and after pregnancy.
Demographics More Susceptible
- Individuals with Diabetes: People with both type 1 and type 2 diabetes are at an increased risk of developing diabetic retinopathy.
- Duration of Diabetes: The risk of diabetic retinopathy rises with the duration of diabetes. Individuals with a longer history of diabetes are more susceptible.
- Poor Blood Sugar Control: Those with poorly controlled blood sugar levels are at a higher risk of developing diabetic retinopathy and experiencing its progression.
- Hypertension and High Cholesterol: Individuals with comorbid conditions, especially high blood pressure and high cholesterol, are more susceptible to diabetic retinopathy.
- Pregnant Women with Diabetes: Pregnancy can exacerbate diabetic retinopathy, making pregnant individuals with diabetes more vulnerable.
Follow-up Care for Adults and Children
For Adults:
- Regular Eye Exams: Continuing regular eye examinations, at least annually or as recommended by the healthcare team, is crucial for monitoring diabetic retinopathy and adjusting treatment plans.
- Blood Sugar Management: Consistent management of blood sugar levels and adherence to prescribed medications are essential for slowing the progression of diabetic retinopathy.
- Lifestyle Modifications: Adopting a healthy lifestyle, including a balanced diet, regular exercise, and smoking cessation, supports overall eye health.
For Children:
- Early Diagnosis: Children with diabetes should have their eyes screened regularly, as diabetic retinopathy can occur even in young individuals.
- Pediatric Ophthalmologist Visits: Regular visits to a pediatric ophthalmologist for monitoring and timely intervention if diabetic retinopathy is detected.
- Education and Support: Parents and caregivers should receive education on the importance of eye care for children with diabetes, including promoting healthy habits.
Conclusion
In conclusion, proactive eye care is vital for individuals with diabetes to prevent, detect, and manage diabetic retinopathy. Early diagnosis and timely treatment can significantly improve outcomes and prevent vision loss. Regular communication with healthcare providers, adherence to recommended screening schedules, and consistent blood sugar control are key components of comprehensive care for diabetic retinopathy.
Through a combination of regular eye examinations, effective diabetes management, and lifestyle modifications, individuals can empower themselves to preserve their vision and mitigate the impact of diabetic retinopathy. Regular follow-up care is essential to monitor the progression of the condition and adjust interventions as needed.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Yes, support groups and organizations dedicated to diabetes and eye health provide valuable resources, shared experiences, and support for individuals and their families managing Diabetic Retinopathy.
Yes, ongoing research is focused on developing new treatments and interventions for Diabetic Retinopathy. Clinical trials and advancements in technology contribute to improving outcomes.
Lifestyle changes, including maintaining a healthy diet, regular exercise, and managing blood sugar levels, can positively impact the management of Diabetic Retinopathy.
In advanced stages, untreated Diabetic Retinopathy can lead to severe vision impairment and even blindness. Timely intervention is crucial to prevent such outcomes.
Pregnancy can influence the progression of Diabetic Retinopathy. Close monitoring and collaboration between healthcare providers are essential for women with diabetes during pregnancy.
Diabetic Retinopathy can develop at any age, but the risk increases with the duration of diabetes. Regular eye check-ups are essential, especially in individuals with long-standing diabetes.
Diabetic Retinopathy can affect both eyes, but the progression may vary. Regular eye examinations help monitor each eye’s health and guide appropriate interventions.
Strict diabetes management, including blood sugar control, blood pressure management, and a healthy lifestyle, can help reduce the risk of Diabetic Retinopathy.
While early stages of Diabetic Retinopathy are manageable, advanced stages may not be reversible. Timely intervention aims to prevent further progression and preserve remaining vision.
Yes, Diabetic Retinopathy can still occur in individuals with well-controlled diabetes. Regular eye examinations remain crucial for early detection and management.
news via inbox
Subscribe here to get latest updates !