Exploring Surgical Approaches for Pterygium Removal
Introduction
Pterygium is a common condition where a triangular-shaped growth of tissue develops on the conjunctiva, usually on the inner corner of the eye. This growth may extend onto the cornea, potentially affecting vision. Pterygium is often associated with chronic exposure to UV light, dust, wind, and other environmental factors. Symptoms can include redness, irritation, foreign body sensation, and in severe cases, vision distortion. Surgical removal is typically recommended when conservative measures such as lubricating eye drops or steroid medications fail to alleviate symptoms or when the pterygium threatens vision.
Understanding Pterygium
Pterygium is characterized by a fibrovascular growth that extends from the conjunctiva onto the cornea. It can cause discomfort, inflammation, and cosmetic concerns. Additionally, if the pterygium encroaches onto the cornea, it may lead to astigmatism and visual disturbances. Pterygium is more common in individuals who spend significant time outdoors, particularly in sunny and windy environments, as UV exposure and ocular irritation are major contributing factors.
Surgical Approaches
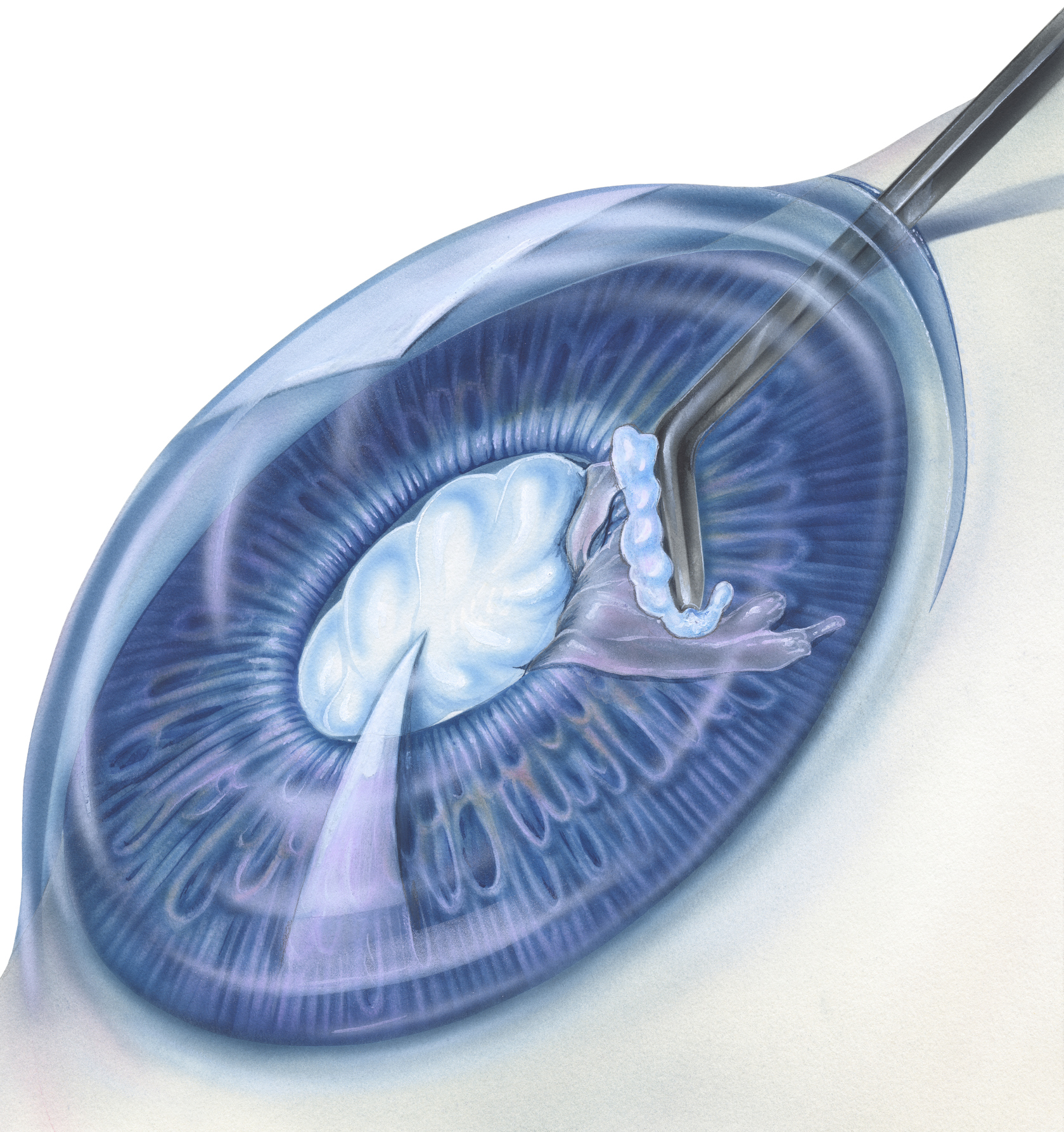
- Conjunctival Autografting: This technique involves removing the pterygium tissue and replacing it with healthy conjunctival tissue harvested from another area of the eye, usually the superior bulbar conjunctiva. The autograft is secured in place with tissue adhesive or sutures. This method helps reduce the risk of pterygium recurrence and promotes better ocular surface healing.
- Amniotic Membrane Transplantation: In this approach, after excising the pterygium, an amniotic membrane graft is used to cover the exposed sclera. The amniotic membrane provides a scaffold for tissue regeneration and reduces inflammation and scarring. It is particularly useful for cases with extensive pterygium involvement or poor ocular surface health.
- Conjunctival Rotation Flap: With this technique, adjacent conjunctival tissue is rotated over the excised pterygium site to cover the bare sclera. Conjunctival rotation flaps are beneficial for large or recurrent pterygia, as they preserve limbal stem cells and help prevent recurrence.
- Mitomycin C (MMC) Therapy: Mitomycin C, an antimetabolite medication, may be applied during or after pterygium surgery to inhibit fibroblast proliferation and reduce the risk of recurrence. MMC is particularly useful in cases with a high risk of pterygium recurrence, such as large or recurrent pterygia or in patients with certain risk factors.
Considerations and Outcomes
Several factors influence the choice of surgical approach and postoperative outcomes:
- Size and Severity: The size, location, and severity of the pterygium determine the complexity of the surgical procedure and the likelihood of recurrence.
- Recurrence Risk: Factors such as previous pterygium recurrence, aggressive growth pattern, and patient demographics influence the choice of surgical technique and the need for adjunctive therapies.
- Patient Factors: Patient age, ocular surface health, presence of comorbidities (e.g., dry eye disease), and lifestyle factors (e.g., outdoor occupation) should be considered when planning pterygium surgery to optimize outcomes and patient satisfaction.
- Postoperative Care: Close postoperative monitoring and diligent care, including topical medications, lubrication, and sun protection, are essential for promoting optimal healing and minimizing complications following pterygium surgery.
Conclusion
Surgical removal of pterygium is a critical intervention for alleviating symptoms, preserving vision, and preventing complications. By understanding the various surgical approaches, their indications, and outcomes, patients and practitioners can collaborate to develop tailored treatment plans that optimize ocular health and comfort. Close postoperative follow-up and adherence to postoperative care instructions are essential for achieving successful outcomes and minimizing the risk of pterygium recurrence.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Recovery time can vary, but most patients can expect to return to normal activities within a week to ten days after surgery. However, full recovery may take several weeks, during which time patients should avoid strenuous activities and follow postoperative care instructions.
During the surgery, patients are typically under local anesthesia, so they do not feel pain. After the procedure, some discomfort and mild pain may occur, which can be managed with prescribed medications and topical eye drops.
Like any surgical procedure, pterygium removal surgery carries some risks, including infection, bleeding, scarring, and recurrence of the pterygium. However, with proper preoperative evaluation and postoperative care, these risks can be minimized.
In most cases, patients do not require an eye patch after pterygium removal surgery. However, your ophthalmologist may recommend using a protective shield or sunglasses to protect the eye from dust, wind, and bright light during the initial healing period.
While surgical removal effectively eliminates the pterygium, there is a risk of recurrence, especially in cases with significant sun exposure or underlying ocular surface conditions. Close follow-up with your ophthalmologist and adherence to postoperative care instructions can help minimize this risk.
The timing of pterygium removal surgery depends on various factors, including the size and severity of the pterygium, symptoms, visual impairment, and patient preferences. Your ophthalmologist will evaluate your individual case and recommend the most appropriate timing for surgery.
While pterygium removal surgery is typically performed under local anesthesia, general anesthesia may be considered for patients who are unable to tolerate local anesthesia or require additional procedures concurrently.
In many cases, pterygium removal surgery is considered a medically necessary procedure and may be covered by health insurance. However, coverage varies depending on your insurance provider, policy terms, and specific circumstances. It’s recommended to check with your insurance company to verify coverage.x
It is not advisable to drive immediately after pterygium removal surgery, as your vision may be temporarily blurred, and you may experience discomfort or sensitivity to light. It’s best to arrange for someone to drive you home after the procedure.
Your ophthalmologist will provide specific guidance on when it’s safe to resume wearing contact lenses after pterygium removal surgery. In general, it’s advisable to wait until the eye has fully healed, which may take several weeks.
news via inbox
Subscribe here to get latest updates !