Granular Cell Tumor Affecting the Eye: A Comprehensive Analysis
Introduction
Granular Cell Tumors (GCTs) are uncommon neoplasms primarily originating from Schwann cells, which form the myelin sheath around peripheral nerves. While these tumors are frequently encountered in cutaneous and subcutaneous tissues, their occurrence in the ocular region is relatively rare. When GCTs affect the eye, they can present unique diagnostic and therapeutic challenges. This detailed article aims to provide an in-depth exploration of granular cell tumors in the eye, covering their etiology, clinical manifestations, diagnostic methods, treatment strategies, and prognostic outlook.
Definition and Background
Granular Cell Tumors are benign lesions characterized by large cells with a granular cytoplasm due to lysosomal granules. These tumors are thought to arise from Schwann cells, which are responsible for nerve myelination. GCTs can be found in various locations, but their appearance in ocular tissues, including the conjunctiva, orbit, eyelids, cornea, and sclera, can impact visual function and ocular health.
Ocular Manifestations
Granular Cell Tumors can affect different parts of the eye, presenting with various clinical features:
- Conjunctiva: GCTs in the conjunctiva often present as a solitary, well-defined mass. They may appear pinkish or yellowish and are usually asymptomatic initially. However, they can cause irritation, a foreign body sensation, or even secondary inflammation if not monitored.
- Orbit: In the orbital region, GCTs may manifest as a palpable mass leading to proptosis (eye bulging) or changes in ocular motility. Symptoms such as eye pain, visual disturbances, or a noticeable bulging of the eye are common. The mass can also cause displacement of the eye or affect adjacent structures.
- Eyelid: Granular cell tumors on the eyelid often present as a firm, nodular growth. They may cause eyelid swelling, discomfort, and alterations in eyelid function. If the tumor is large, it may obstruct vision or lead to cosmetic concerns.
- Cornea and Sclera: Although rare, GCTs affecting the cornea or sclera can cause visual disturbances, such as decreased vision or localized inflammation. These tumors may also present with corneal opacity or scleral thinning, leading to further complications.
Diagnosis
The diagnosis of granular cell tumors affecting the eye involves a multi-faceted approach:
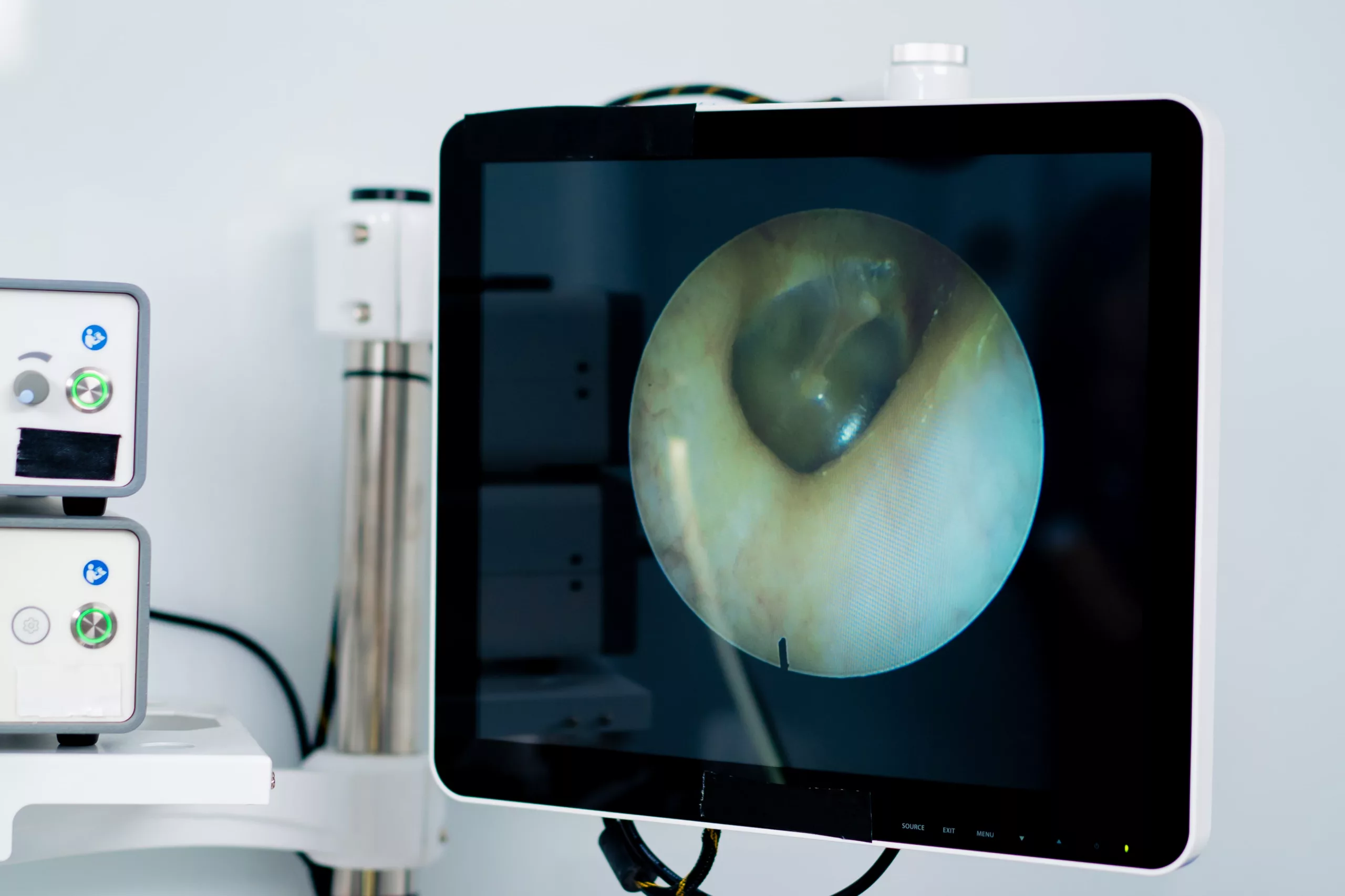
- Clinical Evaluation: A comprehensive eye examination is critical for assessing the tumor’s size, location, and impact on ocular structures. Anterior segment and posterior segment evaluations are essential to understand the extent of the involvement.
- Imaging Studies: Advanced imaging techniques such as B-scan ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) are employed to visualize the tumor’s characteristics and its relationship to surrounding tissues. Imaging helps in planning surgical interventions and assessing for potential metastasis or local invasion.
- Histopathological Examination: A biopsy is crucial for definitive diagnosis. Histological analysis will reveal the characteristic granular cytoplasm of tumor cells. Immunohistochemical staining with markers such as S-100 protein can differentiate GCTs from other tumors with similar presentations.
- Additional Tests: In some cases, molecular genetic studies may be performed to identify specific mutations or genetic markers associated with the tumor, aiding in diagnosis and treatment planning.
Treatment Options
The management of granular cell tumors affecting the eye depends on various factors, including the tumor’s location, size, and potential impact on vision:
- Surgical Excision: The primary treatment for granular cell tumors is complete surgical removal. The goal is to achieve clear margins to minimize the risk of recurrence. Depending on the tumor’s location, various surgical techniques may be used, including local excision or more extensive surgery if necessary.
- Cryotherapy: For certain conjunctival GCTs, cryotherapy (freezing) can be an effective treatment, especially for superficial tumors. Cryotherapy can help in reducing the tumor’s size and facilitating easier removal.
- Radiotherapy: Radiotherapy may be considered for tumors that are difficult to resect or in cases of recurrence. It is typically reserved for specific situations where surgery alone is insufficient or if there is a risk of residual disease.
- Adjunctive Therapies: In some instances, adjunctive therapies such as corticosteroid treatment may be used to manage inflammation or secondary effects associated with the tumor.
Prognosis
Granular cell tumors of the eye are generally benign with a favorable prognosis if detected early and treated appropriately. However, the potential for recurrence exists, particularly if the tumor is not entirely removed or if it was initially misdiagnosed. Long-term follow-up with regular eye examinations is essential to monitor for any signs of recurrence or complications. Prognosis can also depend on the tumor’s location and its impact on surrounding ocular structures.
Conclusion
Granular cell tumors affecting the eye, while rare, pose unique challenges in terms of diagnosis and management. A thorough understanding of their clinical presentation, diagnostic approach, and treatment options is crucial for effective management. Early detection and comprehensive treatment are key to ensuring a positive outcome and preserving ocular function. If you experience any unusual changes in your eyes or symptoms such as discomfort or vision changes, seeking prompt medical evaluation is vital for addressing potential issues and ensuring appropriate care.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Granular cell tumors can occur at any age, but they are most commonly diagnosed in adults between the ages of 30 and 60. However, they can also be seen in children and older adults.
Granular cell tumors are generally considered sporadic and not typically associated with hereditary factors. There is no strong evidence linking them to genetic inheritance or familial predisposition.
Granular cell tumors are usually benign. However, in rare cases, they can exhibit malignant features or undergo malignant transformation. Close monitoring and follow-up are necessary to manage any potential changes.
Granular cell tumors typically have a distinctive granular cytoplasm on histological examination. They often present as well-circumscribed, solitary masses, which can help differentiate them from other types of eye tumors, such as melanoma or lymphoma.
Granular cell tumors of the eye are usually localized and have a low risk of metastasis. However, if the tumor is not treated properly, there is a potential for local invasion or, in very rare cases, distant spread.
Untreated granular cell tumors can lead to complications such as persistent irritation, vision loss, proptosis, and eyelid dysfunction. In severe cases, they may cause significant damage to surrounding ocular structures.
While surgical excision is the primary treatment, some cases, particularly superficial conjunctival GCTs, may be managed with cryotherapy or laser therapy. However, these non-surgical options are generally considered for specific cases where surgery is not feasible or as an adjunct to surgical treatment.
Post-treatment follow-up typically involves regular eye exams to monitor for recurrence or complications. The frequency of follow-ups depends on the tumor’s characteristics and treatment. Follow-ups may include visual assessments and imaging studies.
Imaging studies such as CT, MRI, and B-scan ultrasonography help visualize the extent and location of the tumor, its relationship to surrounding structures, and any potential invasion into adjacent tissues. These studies are crucial for surgical planning and assessing treatment response.
Granular cell tumors are relatively rare compared to other ocular tumors. They are more commonly found in cutaneous and subcutaneous tissues. When they do occur in the eye, they are less frequently diagnosed compared to more common ocular tumors such as conjunctival melanoma or basal cell carcinoma.
news via inbox
Subscribe here to get latest updates !