In the Blink of an Eye: Understanding the Dynamics of Keratitis
Explore the world of keratitis in this article, focusing on when to see a doctor, the impact of this condition, risk factors, potential complications, preventive measures, diagnosis, age groups more susceptible, available treatment options, and a brief conclusion.
Overview of Keratitis
Keratitis is the inflammation of the cornea, the clear front part of the eye covering the iris and the pupil. It can be caused by infections, injuries, or underlying conditions, and if left untreated, it may lead to vision impairment. Understanding the symptoms, causes, consequences, and risk factors associated with keratitis is essential for timely diagnosis and appropriate management.
Symptoms
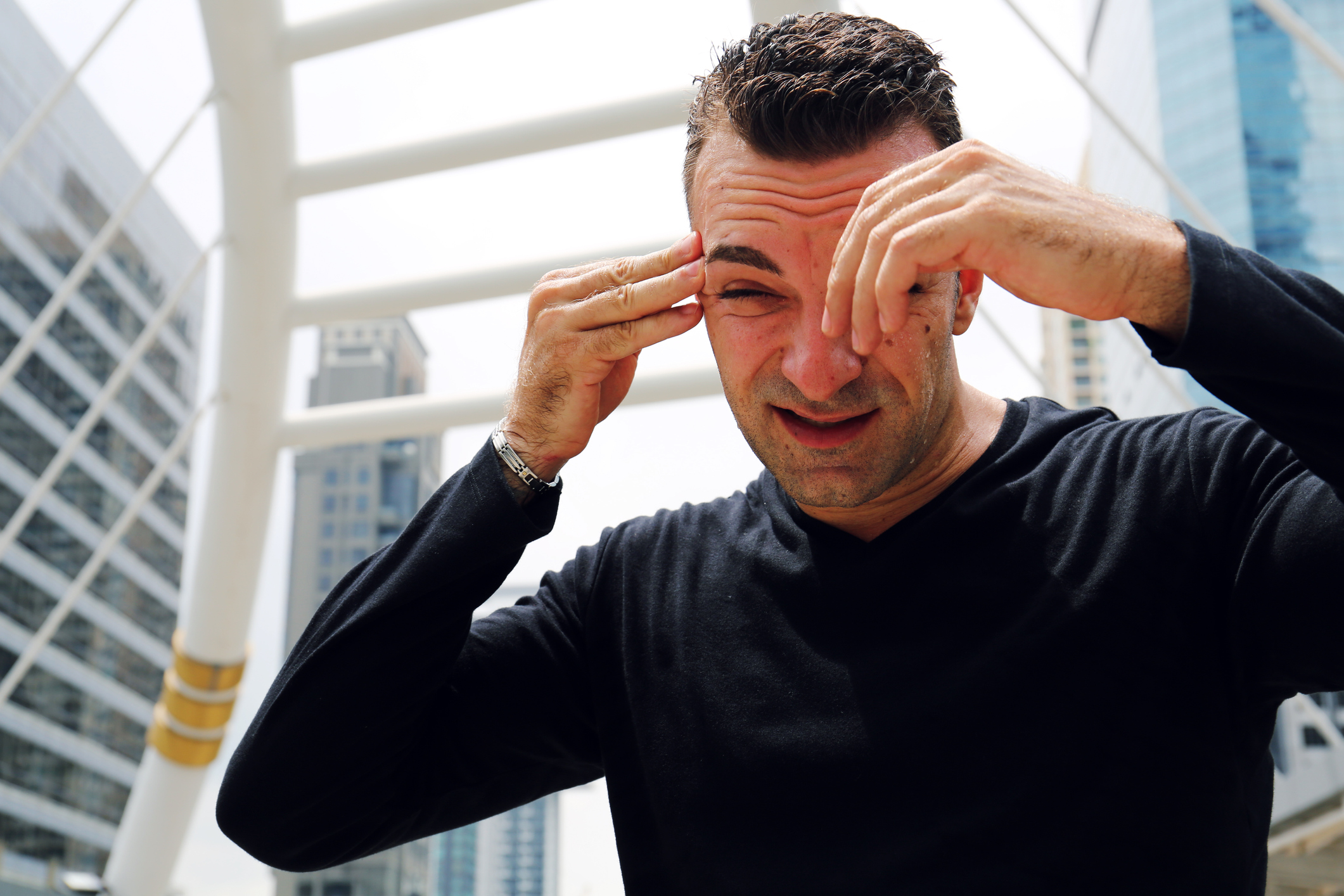
- Eye Pain: Individuals with keratitis often experience pain or discomfort in the affected eye.
- Redness: The eye may appear red and inflamed due to the irritation of the cornea.
- Photophobia: Sensitivity to light, where exposure to light intensifies discomfort.
- Blurry Vision: Vision may become blurred or hazy, affecting clarity.
- Excessive Tearing: Increased tearing or watering of the affected eye.
- Foreign Body Sensation: It may feel as if there is a foreign object in the eye.
- Discharge: In some cases, discharge from the eye, which can be watery, mucous-like, or purulent.
Causes
- Infections: Bacterial, viral, fungal, or parasitic infections can lead to infectious keratitis. Common causative agents include bacteria like Staphylococcus and Pseudomonas, viruses like herpes simplex, and fungi.
- Injury or Trauma: Corneal injuries, scratches, or foreign bodies entering the eye can result in non-infectious keratitis.
- Contact Lens Use: Improper use, hygiene, or extended wear of contact lenses may increase the risk of infectious keratitis, known as contact lens-related keratitis.
- Dry Eye Syndrome: Insufficient tear production or poor tear quality can contribute to non-infectious keratitis.
What Happens Because of the Condition
- Corneal Inflammation: Keratitis leads to inflammation of the cornea, causing redness, pain, and discomfort.
- Blurred Vision: The inflammation and damage to the cornea can result in blurred or hazy vision.
- Sensitivity to Light (Photophobia): Individuals with keratitis often experience increased sensitivity to light, making it uncomfortable to be in well-lit environments.
- Tearing and Discharge: Watery eyes and discharge may occur as the eye attempts to flush out irritants or infectious agents.
- Foreign Body Sensation: Many individuals with keratitis report a feeling of having a foreign body, like sand or grit, in the eye.
Risk Factors
- Contact Lens Use: Improper use, extended wear, or poor hygiene of contact lenses can increase the risk of bacterial, viral, or fungal keratitis.
- Corneal Injury: Any injury or trauma to the cornea, including scratches, cuts, or foreign bodies, can predispose an individual to keratitis.
- Reduced Immune Function: Conditions or medications that suppress the immune system, such as autoimmune diseases or immunosuppressive drugs, can increase susceptibility to keratitis.
- Dry Eye Syndrome: Inadequate tear production or poor tear quality can lead to dry spots on the cornea, making it more susceptible to infection and inflammation.
- Exposure to Irritants: Chemicals, pollutants, or environmental irritants can contribute to the development of keratitis.
- Underlying Eye Conditions: Certain eye conditions, such as blepharitis or conjunctivitis, can increase the risk of developing keratitis.
- Viral Infections: Viruses, such as the herpes simplex virus (HSV) or varicella-zoster virus (VZV), can cause viral keratitis.
Diagnosis
- Clinical Examination: An eye care professional will conduct a thorough examination of the affected eye, assessing symptoms, and looking for signs of inflammation, redness, and changes in the cornea.
- Corneal Culture: If infectious keratitis is suspected, a sample of the corneal tissue or discharge may be collected for laboratory testing to identify the causative organism.
- Visual Acuity Test: Testing visual acuity helps assess the impact of keratitis on vision and determine the need for corrective measures.
- Slit-Lamp Examination: Using a slit lamp, the eye care professional can examine the cornea in detail, checking for abnormalities, lesions, or foreign bodies.
- Fluorescein Staining: This involves applying a special dye to the eye that highlights corneal abrasions, ulcers, or other irregularities during examination under a blue light.
Treatment Options
- Antibiotic or Antifungal Eye Drops: Depending on the cause of keratitis, topical medications containing antibiotics or antifungals may be prescribed to eliminate the infectious agent.
- Corticosteroid Eye Drops: In cases of non-infectious keratitis or when the infection is under control, corticosteroid eye drops may be prescribed to reduce inflammation.
- Oral Medications: Systemic antibiotics or antiviral medications may be prescribed in severe cases or when the infection extends beyond the cornea.
- Pain Medications: Over-the-counter or prescription pain medications may be recommended to manage discomfort.
- Contact Lens Management: If keratitis is related to contact lens use, temporarily discontinuing lens wear and adhering to proper hygiene practices are essential.
Complications
- Corneal Scarring: Severe cases of keratitis can lead to corneal scarring, potentially impacting vision.
- Corneal Ulcer: In some instances, keratitis can progress to the formation of corneal ulcers, requiring intensive treatment.
- Vision Loss: Untreated or inadequately managed keratitis can result in vision loss, especially if complications arise.
- Recurrent Infections: Individuals with a history of keratitis may be at an increased risk of recurrent infections.
Prevention
- Proper Contact Lens Hygiene: Follow proper hygiene practices for contact lens use, including regular cleaning, disinfection, and adherence to recommended wearing schedules.
- Avoiding Eye Trauma: Take precautions to prevent eye injuries, including wearing protective eyewear during activities that pose a risk.
- Regular Eye Examinations: Schedule routine eye exams to monitor eye health and detect potential issues early, especially for individuals using contact lenses.
- Hand Hygiene: Practice good hand hygiene to reduce the risk of transferring infectious agents to the eyes.
- Environmental Protection: Use protective eyewear in environments with potential eye irritants, such as chemicals or debris.
- Addressing Dry Eyes: Manage conditions like dry eye syndrome to maintain proper lubrication and reduce the risk of corneal abrasions.
Medications
- Antibiotic Eye Drops or Ointments: For bacterial keratitis, topical antibiotics are commonly prescribed to eliminate the bacterial infection.
- Antifungal Medications: In cases of fungal keratitis, antifungal eye drops or oral antifungal medications may be prescribed.
- Corticosteroid Eye Drops: In certain situations, corticosteroid eye drops may be used to reduce inflammation associated with non-infectious keratitis. However, these are typically avoided in infectious cases.
- Pain Medications: Over-the-counter or prescription pain medications may be recommended to manage discomfort associated with keratitis.
- Oral Antibiotics or Antivirals: In severe cases or when the infection extends beyond the cornea, oral antibiotics or antivirals may be prescribed.
When to See a Doctor
- Eye Pain or Discomfort: If you experience persistent eye pain, discomfort, or a foreign body sensation.
- Redness or Swelling: Significant redness or swelling of the eye.
- Changes in Vision: Any sudden changes in vision, including blurriness or increased sensitivity to light.
- Eye Trauma: In case of eye injuries, scratches, or exposure to foreign bodies.
- Contact Lens-related Symptoms: If you wear contact lenses and experience symptoms such as redness, pain, or discharge.
- Symptoms in Children: Children may not always communicate their symptoms clearly, so it’s important to seek professional evaluation for any signs of eye discomfort, redness, or changes in behavior related to vision.
Demographics More Susceptible
- Contact Lens Wearers: Individuals who wear contact lenses, especially if hygiene practices are not followed rigorously, are at a higher risk of keratitis.
- People with Compromised Immune Systems: Those with conditions or medications that weaken the immune system may be more susceptible to infections, including keratitis.
- Outdoor Workers or Enthusiasts: People who work or spend significant time outdoors, particularly in dusty or windy conditions, may be at a higher risk of corneal injuries that can lead to keratitis.
- Individuals with Dry Eye Syndrome: Reduced tear production or poor tear quality can increase the risk of corneal abrasions, making individuals with dry eye syndrome more susceptible.
Follow-up Care for Adults and Children
For Adults:
- Adherence to Medications: Follow the prescribed medication regimen as directed by the healthcare provider.
- Regular Follow-up Appointments: Attend follow-up appointments to monitor the progress of treatment and ensure proper healing.
- Contact Lens Practices: If contact lens-related, adhere to recommended practices and schedules, and attend regular eye check-ups.
For Children:
- Parental Observation: Parents should closely observe and communicate with their children to identify any signs of eye discomfort or changes in vision.
- Adherence to Treatment Plan: Ensure that children adhere to the prescribed medication regimen and follow any recommendations for eye care.
- Communication with School: If applicable, communicate with teachers or school staff about the child’s condition and any necessary accommodations.
Conclusion
Keratitis requires prompt attention and appropriate management to prevent complications and preserve vision. Seeking medical care at the first signs of symptoms is crucial. Adherence to prescribed medications, regular follow-up appointments, and preventive measures are essential components of successful treatment. Both adults and children should be vigilant about eye health, and any concerns should be addressed promptly. With proper care and timely intervention, individuals with keratitis can often achieve positive outcomes and minimize the impact on their vision.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
In some cases, autoimmune conditions like dry eye syndrome or Sjögren’s syndrome can contribute to Keratitis. Managing the underlying autoimmune condition is essential for eye health.
Contaminated or expired eye makeup can introduce bacteria and increase the risk of Keratitis. Using clean brushes, avoiding expired products, and removing makeup before sleep are important precautions.
Warm and humid climates may slightly increase the risk of Keratitis, especially fungal types. However, good hygiene practices and proper eye care are essential in all climates.
Yes, swimming with contact lenses increases the risk of infection, including Acanthamoeba Keratitis. Removing lenses before swimming and using waterproof goggles are recommended.
Fungal Keratitis prevention involves avoiding contact with contaminated substances, practicing good eye hygiene, and using sterile solutions for contact lenses.
Prolonged use of certain eye drops, especially those containing preservatives, may contribute to Keratitis. Following recommended usage and consulting with an eye care professional is important.
Viral Keratitis, especially caused by herpes simplex virus, may have recurring episodes. Managing triggers and following prescribed antiviral medications help control recurrence.
With prompt and appropriate treatment, many cases of Keratitis can be resolved without permanent vision loss. However, severe or untreated cases may lead to complications affecting vision.
Bacterial Keratitis can be contagious, especially if it results from poor hygiene or contact with contaminated substances. Following proper hygiene and avoiding shared items help prevent spread.
Yes, improper contact lens hygiene or extended wear can increase the risk of contact lens-related Keratitis. Following hygiene guidelines and regular check-ups are crucial for contact lens users.
news via inbox
Subscribe here to get latest updates !