Keratoconus: A Guide to Symptoms, Causes, and Care
Embark on a journey to understand keratoconus, a progressive eye condition characterized by the thinning and bulging of the cornea. This article serves as your guide, providing insights into the causes of keratoconus, common symptoms, and available treatment options. Delve into risk factors, complications, preventive measures, and the importance of seeking timely medical attention for this corneal shape-changing disorder.
Overview of Keratoconus
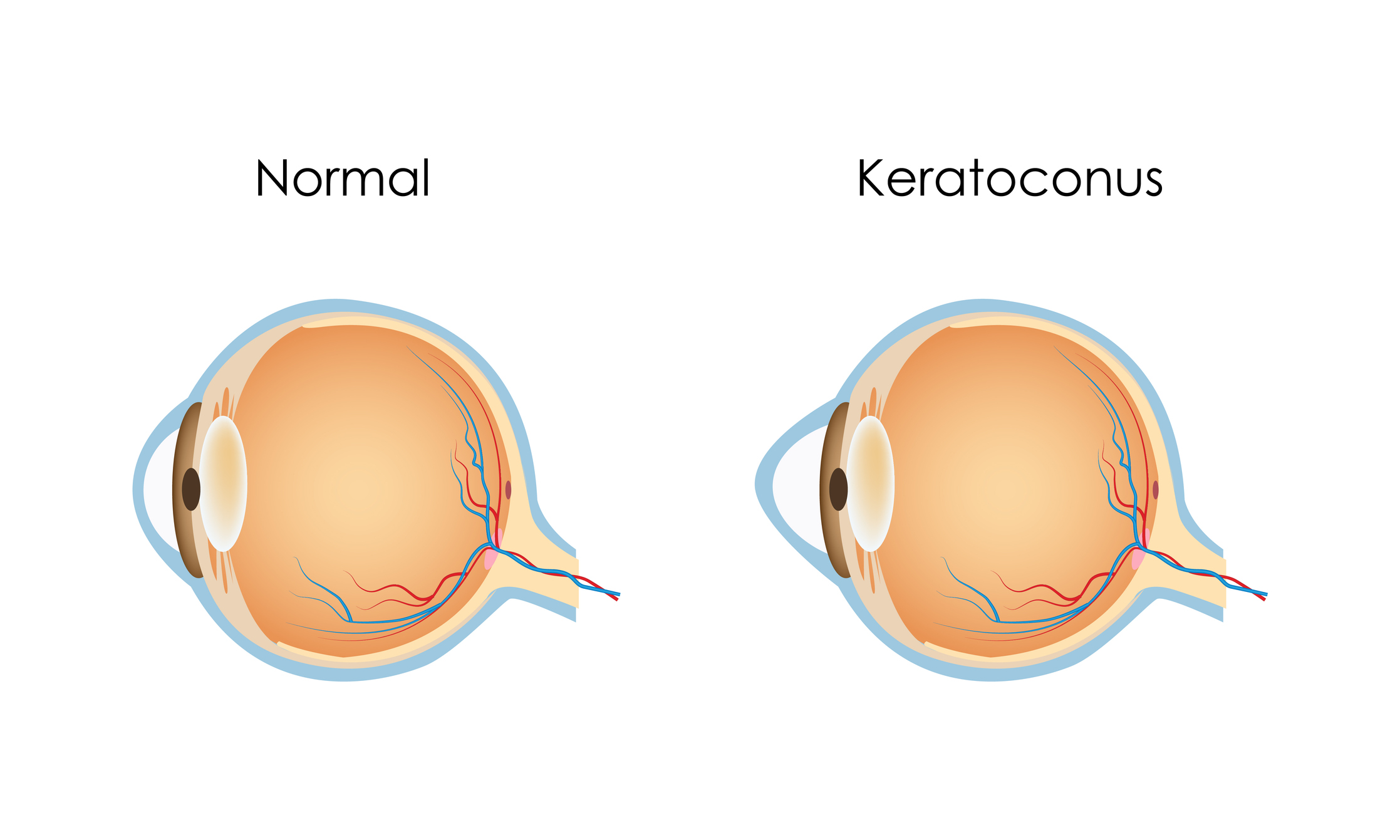
Keratoconus is a progressive eye disorder that affects the cornea, the clear, dome-shaped front surface of the eye. In individuals with keratoconus, the cornea gradually thins and bulges into a cone-like shape, leading to distorted vision. This condition can result in significant visual impairment and may require special corrective measures, such as rigid gas permeable contact lenses or, in severe cases, surgical interventions.
Symptoms
- Blurred or Distorted Vision: Progressive thinning and bulging of the cornea lead to distorted or blurred vision.
- Increased Sensitivity to Light (Photophobia): The altered shape of the cornea may result in heightened sensitivity to light.
- Frequent Changes in Prescription Glasses or Contacts: Due to the changing corneal shape, individuals may experience frequent changes in prescription glasses or contact lenses.
- Astigmatism: Astigmatism becomes more pronounced as the cornea loses its regular shape.
Causes
- Genetic Factors: There is a genetic predisposition, and a family history of keratoconus may increase the risk.
- Biomechanical Changes: Weakening of the corneal tissue and alterations in its structural integrity contribute to the condition.
- Enzyme Abnormalities: Changes in the balance of enzymes responsible for maintaining corneal structure can lead to thinning.
What Happens Because of the Condition
- Corneal Thinning: Keratoconus causes progressive thinning of the cornea, leading to its conical shape.
- Corneal Bulging: The weakened cornea bulges outward, altering the refractive properties of the eye.
- Vision Distortion: Irregular corneal shape results in distorted vision, astigmatism, and myopia.
Risk Factors
- Family History: Having a family member with keratoconus increases the risk.
- Eye Rubbing: Constant and vigorous eye rubbing may contribute to the progression of keratoconus.
- Underlying Conditions: Conditions like atopic diseases (eczema, asthma) may be associated with keratoconus.
Diagnosis
- Corneal Topography: A non-invasive mapping of the cornea’s shape helps diagnose irregularities characteristic of keratoconus.
- Slit-Lamp Examination: A high-powered microscope (slit lamp) allows a detailed examination of the cornea’s structure.
- Refraction Test: Determines the extent of vision impairment and helps in prescribing corrective lenses.
Treatment Options
- Glasses or Contact Lenses: In the early stages, corrective lenses may be sufficient to address vision problems.
- Custom Contact Lenses: Specially designed contact lenses, such as rigid gas permeable or scleral lenses, can improve vision in more advanced cases.
- Corneal Cross-Linking: A procedure involving the application of ultraviolet light and riboflavin eye drops to strengthen the corneal collagen.
- Intacs: Implantation of small, semi-circular devices into the cornea to reshape and provide better structural support.
- Intraocular Rings (ICRs): Surgical placement of rings within the cornea to reshape its surface.
- Corneal Transplant (Penetrating Keratoplasty or DALK): In severe cases, a corneal transplant may be considered.
- Phakic Intraocular Lens (IOL) Implantation: In certain cases, implanting a lens in addition to the natural lens inside the eye may be an option.
Complications
- Progressive Vision Loss: Without proper management, keratoconus can lead to progressive and significant vision impairment.
- Corneal Scarring: Advanced cases may result in corneal scarring, further contributing to visual distortion.
- Contact Lens Intolerance: As the cornea undergoes changes, individuals with keratoconus may develop intolerance to standard contact lenses.
Prevention
- Regular Eye Exams: Regular eye examinations, especially for individuals with a family history of keratoconus, can aid in early detection and intervention.
- Avoiding Eye Rubbing: Minimizing eye rubbing, particularly in individuals prone to atopic diseases, may help reduce the risk of keratoconus progression.
Medications
- Riboflavin (Vitamin B2) Eye Drops: Used in conjunction with ultraviolet light during corneal cross-linking to strengthen the corneal collagen.
- Prescription Eye Drops: In some cases, eye drops may be prescribed to address discomfort or manage associated conditions.
When to See a Doctor
- Vision Changes: Any sudden or significant changes in vision, especially blurriness or distortion, warrant immediate attention.
- Frequent Changes in Prescription: Individuals experiencing frequent changes in eyeglass or contact lens prescriptions should consult an eye care professional.
- Eye Discomfort or Pain: Persistent eye discomfort, pain, or light sensitivity should be promptly evaluated by a doctor.
Demographics More Susceptible
- Age and Genetics: Keratoconus often manifests in adolescence or early adulthood, and there is a genetic predisposition, making individuals with a family history more susceptible.
- Atopic Diseases: Those with atopic diseases like eczema or asthma may have a higher risk of developing keratoconus.
- Eye Rubbing: Constant and vigorous eye rubbing, often seen in individuals with allergies, may contribute to the progression of keratoconus.
Follow-up Care for Adults and Children
- Regular Monitoring: Individuals with keratoconus require regular monitoring by an eye care professional to assess progression and adjust treatment plans accordingly.
- Children:
- Pediatric Ophthalmologist: Children with keratoconus should receive ongoing care from a pediatric ophthalmologist.
- Educational Support: Providing educational support for children with visual impairment to ensure their academic success.
- Adults:
- Regular Eye Exams: Frequent eye examinations for adults to monitor changes in vision and corneal health.
- Adaptation to Treatment: Ensuring that adults are adapting well to prescribed treatments, such as contact lenses or post-surgical care.
Conclusion
Keratoconus demands vigilant monitoring and proactive management to address complications and preserve vision. Timely intervention, whether through corrective lenses, corneal cross-linking, or surgical procedures, plays a pivotal role in maintaining optimal eye health. Collaboration with eye care professionals and adherence to recommended follow-up care are essential for individuals with keratoconus to navigate potential complications and achieve the best possible visual outcomes.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
LASIK is generally not recommended for keratoconus, but other surgical options may be considered in certain cases.
While treatment can manage the condition and prevent progression, it does not reverse the corneal changes.
There is a genetic component, and individuals with a family history of keratoconus have a higher risk.
Poorly fitted or rigid contact lenses may exacerbate keratoconus symptoms, but specialized lenses can provide relief.
Corneal cross-linking can halt the progression of keratoconus, but additional treatments may still be needed to correct vision.
In the early stages, regular eyeglasses may be used, but as the condition progresses, specialized lenses may be necessary.
Keratoconus itself is not typically painful, but it can cause discomfort due to changes in vision.
Yes, keratoconus can affect one or both eyes, but it often progresses more rapidly in one eye.
Keratoconus often starts during adolescence or early adulthood, but it can develop at any age.
Keratoconus is considered relatively uncommon, affecting about 1 in 2,000 people.
news via inbox
Subscribe here to get latest updates !