Map-Dot-Fingerprint Dystrophy: A Comprehensive Guide
Introduction
Map-Dot-Fingerprint Dystrophy (MDFD), also known as Epithelial Basement Membrane Dystrophy (EBMD), is a common corneal dystrophy affecting the epithelial layer of the cornea. This condition is characterized by abnormalities in the basement membrane, leading to a variety of visual symptoms and discomfort. Understanding the intricacies of MDFD is crucial for proper diagnosis and management. This article provides an in-depth exploration of Map-Dot-Fingerprint Dystrophy, including its etiology, clinical presentation, diagnosis, treatment options, and prognosis.
What is Map-Dot-Fingerprint Dystrophy?
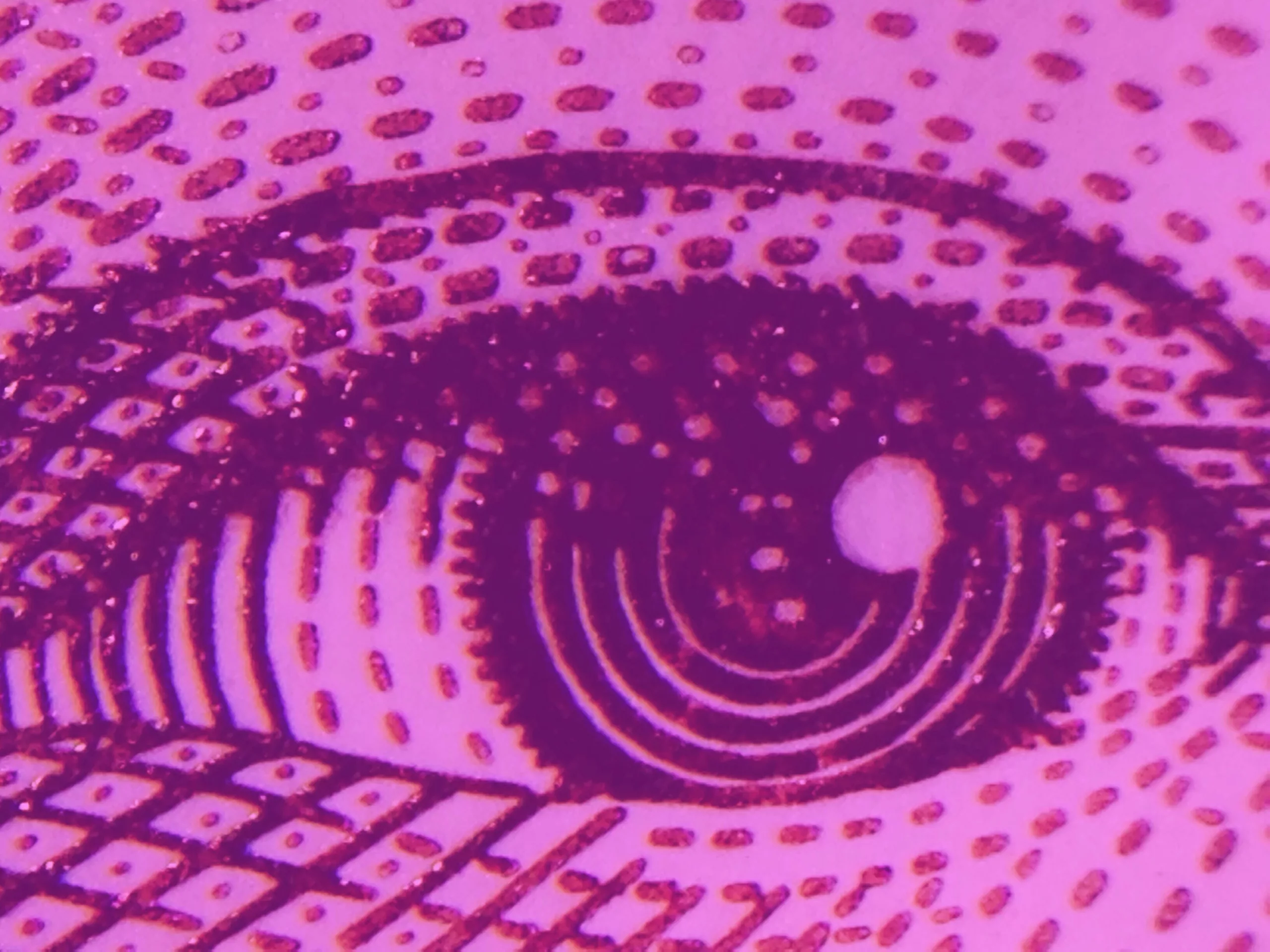
Map-Dot-Fingerprint Dystrophy is a disorder of the corneal epithelium, the outermost layer of the cornea. It is characterized by a range of abnormal findings, including map-like patterns, dot-like opacities, and fingerprint-like lines in the epithelial layer. These changes occur due to irregularities in the epithelial basement membrane, which affects the corneal surface’s integrity and function.
Etiology and Pathophysiology
The exact cause of Map-Dot-Fingerprint Dystrophy is not fully understood, but it is believed to have a genetic basis. Mutations in genes responsible for corneal epithelial development and maintenance may contribute to the condition. The dystrophy is typically inherited in an autosomal dominant pattern, meaning a single copy of the altered gene in each cell is sufficient to cause the disorder.
The primary pathophysiological feature of MDFD is the abnormal deposition of extracellular matrix components in the basement membrane of the corneal epithelium. This leads to the formation of irregular epithelial patterns and areas of disorganized cellular attachment, causing the characteristic map-like and fingerprint-like appearances.
Clinical Presentation
Map-Dot-Fingerprint Dystrophy can present with a range of symptoms and findings:
- Visual Symptoms: Patients with MDFD may experience blurred vision, especially upon waking, due to epithelial irregularities and potential corneal edema. Visual acuity can fluctuate, and symptoms may worsen with age or during periods of eye strain.
- Corneal Findings: On examination, the cornea may exhibit map-like lines, dot-like opacities, and fingerprint-like patterns. These findings are typically observed using slit-lamp microscopy, which allows for detailed visualization of the corneal surface.
- Discomfort: Some patients report ocular discomfort, including irritation, burning, or foreign body sensation. In severe cases, recurrent corneal erosions may occur, leading to episodes of acute pain and vision disturbances.
Diagnosis
The diagnosis of Map-Dot-Fingerprint Dystrophy is primarily clinical, based on the characteristic appearance of the corneal epithelium observed through slit-lamp examination. Additionally, the following diagnostic methods may be used:
- Slit-Lamp Examination: This is the cornerstone of diagnosis, allowing the clinician to visualize the characteristic epithelial patterns and assess the severity of the dystrophy.
- Corneal Topography: This imaging technique helps to map out the corneal surface and identify any irregularities in curvature or elevation associated with MDFD.
- Confocal Microscopy: This advanced imaging modality provides detailed visualization of corneal epithelial layers and can help in identifying changes in the basement membrane.
Treatment Options
Treatment for Map-Dot-Fingerprint Dystrophy is tailored to the severity of symptoms and the impact on the patient’s vision. Management strategies include:
- Symptomatic Relief: For mild cases, over-the-counter lubricating eye drops or ointments can provide relief from dryness and discomfort. Artificial tears help to maintain moisture on the corneal surface and reduce symptoms.
- Hypertonic Saline Solutions: These solutions can be used to reduce corneal swelling and improve visual clarity. They work by drawing fluid out of the corneal tissue.
- Debridement: In cases where recurrent corneal erosions occur, a procedure called debridement may be performed. This involves removing damaged epithelial cells to promote healing and reduce the likelihood of further erosions.
- Epithelial Patching: In more severe cases, a technique called epithelial patching, which involves placing a bandage contact lens on the eye, can aid in healing and protect the corneal surface.
- Phototherapeutic Keratectomy (PTK): For persistent and severe cases, PTK may be recommended. This laser-based procedure removes irregular epithelial layers and promotes a smoother corneal surface.
Prognosis
The prognosis for Map-Dot-Fingerprint Dystrophy is generally good. While the condition can cause discomfort and visual disturbances, many patients experience relief with appropriate management. The dystrophy tends to stabilize over time, and symptoms often improve with treatment. Regular follow-up with an ophthalmologist is essential to monitor the condition and adjust treatment as needed.
Conclusion
Map-Dot-Fingerprint Dystrophy (Epithelial Basement Membrane Dystrophy) is a common corneal condition characterized by distinctive epithelial abnormalities. Understanding the etiology, clinical presentation, and treatment options is crucial for effective management and improving patient outcomes. With appropriate care and treatment, individuals with MDFD can achieve significant relief from symptoms and maintain good visual function. If you suspect you have MDFD or are experiencing symptoms, consult an ophthalmologist for a comprehensive evaluation and personalized treatment plan.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Map-Dot-Fingerprint Dystrophy is primarily caused by genetic mutations affecting the corneal epithelial basement membrane. It is typically inherited in an autosomal dominant pattern.
MDFD is one of the most common corneal dystrophies, affecting a significant number of individuals, with a prevalence that varies across different populations.
Symptoms of MDFD often begin in late adolescence or early adulthood, but the condition can be diagnosed at any age.
Since MDFD is a genetic condition, it cannot be prevented. However, early diagnosis and management can help control symptoms and improve quality of life.
Yes, MDFD is hereditary and can be passed from one generation to the next. It follows an autosomal dominant inheritance pattern, meaning a single copy of the altered gene can cause the condition.
Symptoms of recurrent corneal erosions may include sudden pain, tearing, blurred vision, and a foreign body sensation in the eye. These erosions occur when the epithelial layer of the cornea fails to adhere properly.
While lifestyle changes cannot cure MDFD, maintaining good ocular hygiene, using lubricating eye drops regularly, and avoiding environmental irritants can help manage symptoms.
Vision may fluctuate, especially if symptoms worsen or recurrent corneal erosions occur. With appropriate treatment, most patients can achieve stable and satisfactory vision.
In rare cases, persistent corneal damage from recurrent erosions may lead to complications such as scarring or reduced visual acuity. Regular follow-up with an ophthalmologist is important to prevent complications.
Advances in treatment include improved laser techniques like Phototherapeutic Keratectomy (PTK) and ongoing research into gene therapies. Consulting with an ophthalmologist can provide information on the latest treatment options.
news via inbox
Subscribe here to get latest updates !