Navigating the Causes and Symptoms of Pink Eye
Dive into the topic of conjunctivitis in this article, focusing on when to see a doctor, the impact of this condition, risk factors, potential complications, preventive measures, diagnosis, age groups more susceptible, available treatment options, and a brief conclusion.
Overview of Conjunctivitis
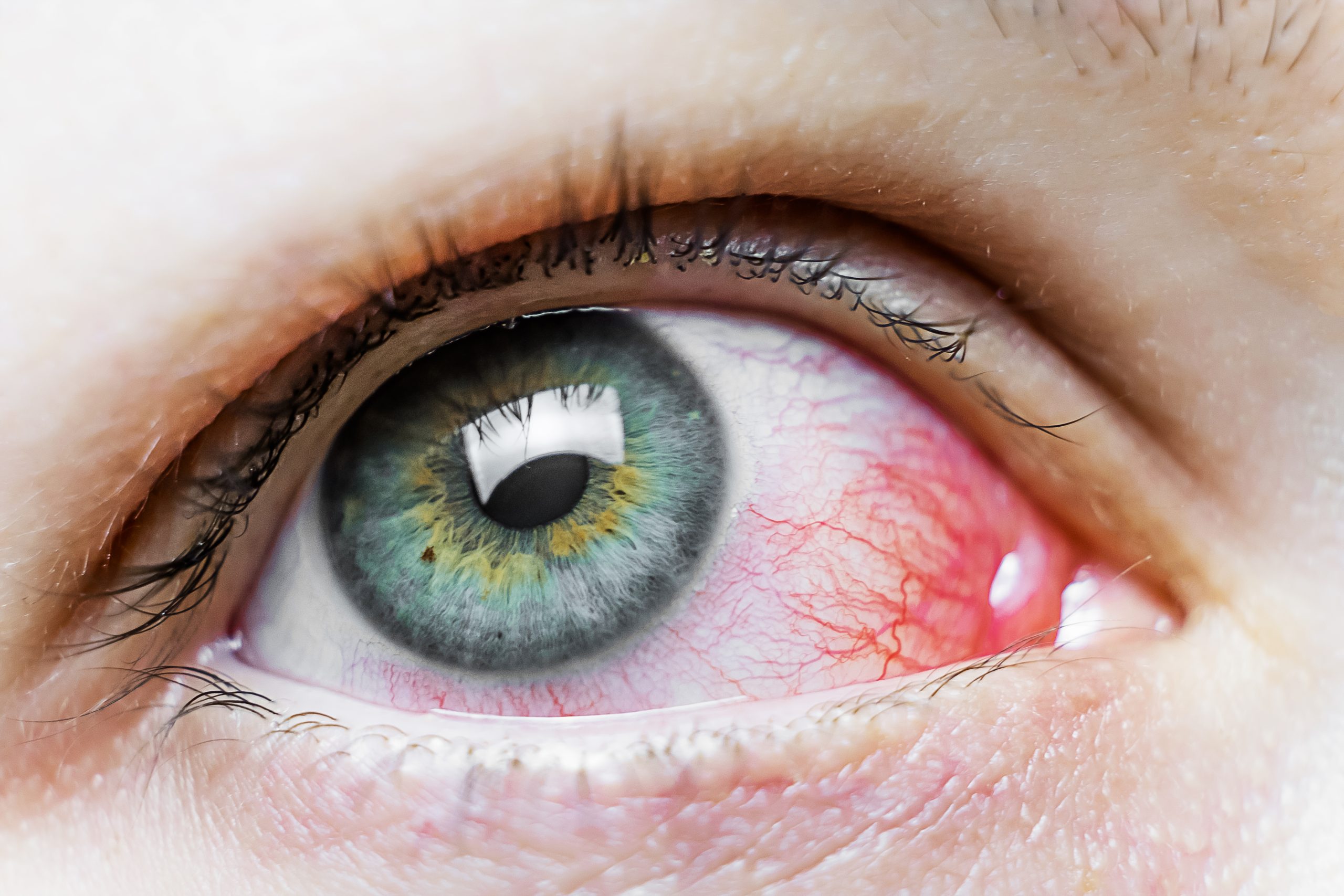
Conjunctivitis, commonly known as pink eye, is the inflammation of the conjunctiva, the thin and transparent membrane covering the white part of the eye and the inner surface of the eyelids. This condition can be caused by various factors, including infections, allergens, or irritants. Understanding the symptoms, causes, and consequences of conjunctivitis is crucial for effective management and appropriate treatment.
Symptoms
- Redness: The whites of the eyes may appear pink or red.
- Watery Eyes: Excessive tearing or watering of the eyes.
- Itching: Persistent itching or irritation in the eyes.
- Discharge: Discharge from the eyes, which can be clear, yellow, or greenish.
- Sensitivity to Light: Increased sensitivity to light (photophobia).
- Gritty Sensation: Feeling of having something gritty or foreign in the eyes.
- Swelling: Swelling of the conjunctiva, making the eyes appear puffy.
Causes
- Viral Infections: Viruses, such as adenovirus, are a common cause of viral conjunctivitis. It is highly contagious and often associated with upper respiratory infections.
- Bacterial Infections: Bacterial conjunctivitis is caused by bacteria, such as Staphylococcus or Streptococcus. It can result from poor hygiene or contact with contaminated surfaces.
- Allergies: Allergic conjunctivitis is triggered by allergens such as pollen, pet dander, or dust mites.
- Irritants: Exposure to irritants like smoke, pollution, or chemicals can lead to irritant conjunctivitis.
- Contact Lens Use: Improper lens care or extended wear of contact lenses can contribute to conjunctivitis.
What Happens Because of the Condition
- Inflammation: The conjunctiva becomes inflamed, leading to the characteristic redness and swelling.
- Increased Tear Production: The eyes may produce excess tears as a response to the irritation.
- Discharge: Conjunctivitis often results in the production of a discharge, which can vary in color and consistency depending on the underlying cause.
- Photophobia: Sensitivity to light may occur, making it uncomfortable to be in well-lit environments.
- Vision Disturbance: While conjunctivitis itself doesn’t typically cause severe vision problems, the associated symptoms like discharge and tearing can temporarily blur vision.
Risk Factors
- Close Contact with Infected Individuals: Conjunctivitis, especially the viral and bacterial forms, is highly contagious. Close contact with someone who has conjunctivitis increases the risk of transmission.
- Poor Hygiene Practices: Inadequate handwashing and poor hygiene, especially in crowded or shared spaces, can contribute to the spread of infectious conjunctivitis.
- Allergen Exposure: Individuals with a history of allergies or exposure to allergens, such as pollen, pet dander, or dust mites, are at a higher risk of developing allergic conjunctivitis.
- Contact Lens Wear: Improper cleaning, extended wear, or using contaminated solutions for contact lenses increases the risk of developing contact lens-related conjunctivitis.
- Occupational Exposures: People working in environments with airborne irritants, pollutants, or chemicals may be at an increased risk of irritant conjunctivitis.
- Underlying Health Conditions: Individuals with pre-existing health conditions, such as autoimmune disorders or conditions that compromise the immune system, may be more susceptible to conjunctivitis.
Diagnosis
- Clinical Examination: A healthcare professional examines the eyes for characteristic signs, including redness, swelling, discharge, and other symptoms associated with conjunctivitis.
- Patient History: Gathering information about recent illness, exposure to irritants or allergens, and contact with infected individuals helps in identifying the potential cause.
- Laboratory Tests: In cases where the cause is uncertain, laboratory tests, such as conjunctival swabs or cultures, may be performed to identify the specific pathogen (bacteria or virus).
Treatment Options
- Viral Conjunctivitis:
- Self-limiting: Most cases resolve on their own without specific treatment.
- Symptomatic Relief: Lubricating eye drops or cold compresses can provide relief from symptoms.
- Bacterial Conjunctivitis:
- Antibiotic Eye Drops or Ointments: Topical antibiotics are prescribed to treat bacterial infections.
- Oral Antibiotics: In severe cases, oral antibiotics may be recommended.
- Allergic Conjunctivitis:
- Allergen Avoidance: Identifying and avoiding triggers.
- Antihistamines: Oral or topical antihistamines can help manage symptoms.
- Irritant Conjunctivitis:
- Irritant Avoidance: Removing or minimizing exposure to the irritating substance.
- Artificial Tears: Lubricating eye drops may help soothe irritation.
Complications
- Corneal Involvement: Severe or prolonged cases of conjunctivitis can lead to corneal complications, including keratitis.
- Chronic Conjunctivitis: Some cases, particularly chronic allergic conjunctivitis, can lead to long-term inflammation and discomfort.
- Vision Disturbance: While uncommon, severe cases or complications may temporarily affect vision.
- Spread to Other People: Infectious forms of conjunctivitis can be highly contagious, leading to the spread of the condition to family members, colleagues, or others in close proximity.
- Recurrence: Individuals with a history of conjunctivitis, especially allergic or recurrent forms, may experience repeated episodes.
Prevention
- Hand Hygiene: Wash hands regularly with soap and water, especially after contact with surfaces in public places, to prevent the spread of infectious conjunctivitis.
- Avoid Touching Eyes: Refrain from touching or rubbing the eyes, as this can introduce irritants or infectious agents.
- Personal Items: Avoid sharing personal items, such as towels, pillows, or eye makeup, to prevent the transmission of conjunctivitis.
- Contact Lens Hygiene: Follow proper hygiene practices for contact lens use, including cleaning, disinfection, and regular replacement to minimize the risk of contact lens-related conjunctivitis.
- Allergen Avoidance: Identify and minimize exposure to allergens that trigger allergic conjunctivitis, such as pollen, pet dander, or dust mites.
- Protective Eyewear: Wear protective eyewear in environments where irritants, pollutants, or chemicals may be present to prevent irritant conjunctivitis.
Medications
- Antibiotic Eye Drops or Ointments: Prescribed for bacterial conjunctivitis to eliminate the bacterial infection.
- Antihistamines: Oral or topical antihistamines can help manage symptoms in cases of allergic conjunctivitis.
- Artificial Tears: Lubricating eye drops may provide relief from dryness and discomfort associated with various forms of conjunctivitis.
- Vasoconstrictor Eye Drops: Used to reduce redness in certain cases, but these should be used cautiously and under the guidance of a healthcare professional.
When to See a Doctor
- Persistent Symptoms: If symptoms persist or worsen despite home care measures.
- Severe Pain or Vision Changes: Immediate medical attention is warranted if there is severe eye pain, sudden vision changes, or symptoms suggestive of a more serious condition.
- Contact Lens-related Symptoms: Individuals wearing contact lenses who experience symptoms like redness, pain, or discharge should see a doctor promptly.
- Symptoms in Children: Parents should seek medical advice for children exhibiting symptoms such as eye redness, tearing, or rubbing.
Demographics More Susceptible
- Children: Children, due to close contact in school or daycare settings, may be more susceptible to infectious conjunctivitis.
- Contact Lens Wearers: Individuals who wear contact lenses, especially those not following proper hygiene practices, are at an increased risk of developing conjunctivitis.
- Allergy Sufferers: Individuals with a history of allergies are more prone to allergic conjunctivitis.
- Occupational Exposure: Those working in environments with airborne irritants or chemicals may be more susceptible to irritant conjunctivitis.
Follow-up Care for Adults and Children
For Adults:
- Medication Adherence: Adhere to the prescribed medication regimen as directed by the healthcare provider.
- Follow-up Appointments: Attend follow-up appointments as recommended to monitor the progress of treatment.
- Contact Lens Practices: If contact lens-related, follow recommended practices and schedules, and attend regular eye check-ups.
For Children:
- Parental Observation: Parents should closely observe and communicate with their children to identify any signs of eye discomfort or changes in vision.
- Adherence to Treatment Plan: Ensure that children adhere to the prescribed medication regimen and follow any recommendations for eye care.
- Communication with School: If applicable, communicate with teachers or school staff about the child’s condition and any necessary accommodations.
Conclusion
Conjunctivitis, while often a self-limiting condition, requires appropriate care and preventive measures to minimize its impact. Adhering to good hygiene practices, seeking timely medical attention when necessary, and addressing risk factors contribute to effective prevention and management. Regular follow-up care ensures that treatment is on track and complications are promptly addressed. By taking preventive measures and seeking timely care, both adults and children can navigate conjunctivitis with minimal discomfort and a swift recovery.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Over-the-counter eye drops may provide relief for certain types of Conjunctivitis, but consulting with an eye care professional is crucial for an accurate diagnosis and appropriate treatment.
Conjunctivitis itself typically does not cause permanent vision loss. Proper management and timely treatment are essential to prevent complications that could affect vision.
It is advisable to avoid wearing eye makeup during Conjunctivitis to prevent further irritation and contamination. Discarding old makeup and practicing good hygiene are crucial.
Yes, swimming in pools with inadequate chlorine levels may increase the risk of Conjunctivitis. Wearing swim goggles and avoiding opening eyes underwater can help prevent irritation.
Yes, newborns can acquire Conjunctivitis during delivery if the mother has a sexually transmitted infection. Applying preventive eye ointment to newborns helps reduce the risk.
Yes, during allergy seasons, avoiding allergens, using antihistamine eye drops, and practicing good eye hygiene can help prevent or alleviate allergic Conjunctivitis.
Bacterial Conjunctivitis is often more contagious than viral Conjunctivitis. However, both types require precautions to prevent transmission, such as frequent handwashing and avoiding shared items.
Yes, improper contact lens hygiene or extended wear can increase the risk of contact lens-related Conjunctivitis. Following hygiene guidelines and regular check-ups are crucial for contact lens users.
While rare, viral Conjunctivitis can sometimes be associated with respiratory infections. Proper hygiene practices help prevent the spread of the virus to other areas.
No, Conjunctivitis can also result from allergies, irritants, or underlying health conditions. Identifying the specific cause helps determine the most effective treatment.
news via inbox
Subscribe here to get latest updates !