Navigating the Essentials of Retinal Hemorrhage
Retinal hemorrhage, the leakage of blood into the retina, can impact vision and signal underlying health issues. This article aims to provide an accessible guide to Retinal Hemorrhage, covering symptoms, causes, when to seek medical attention, risk factors, prevention strategies, available treatments, and follow-up care for both adults and children.
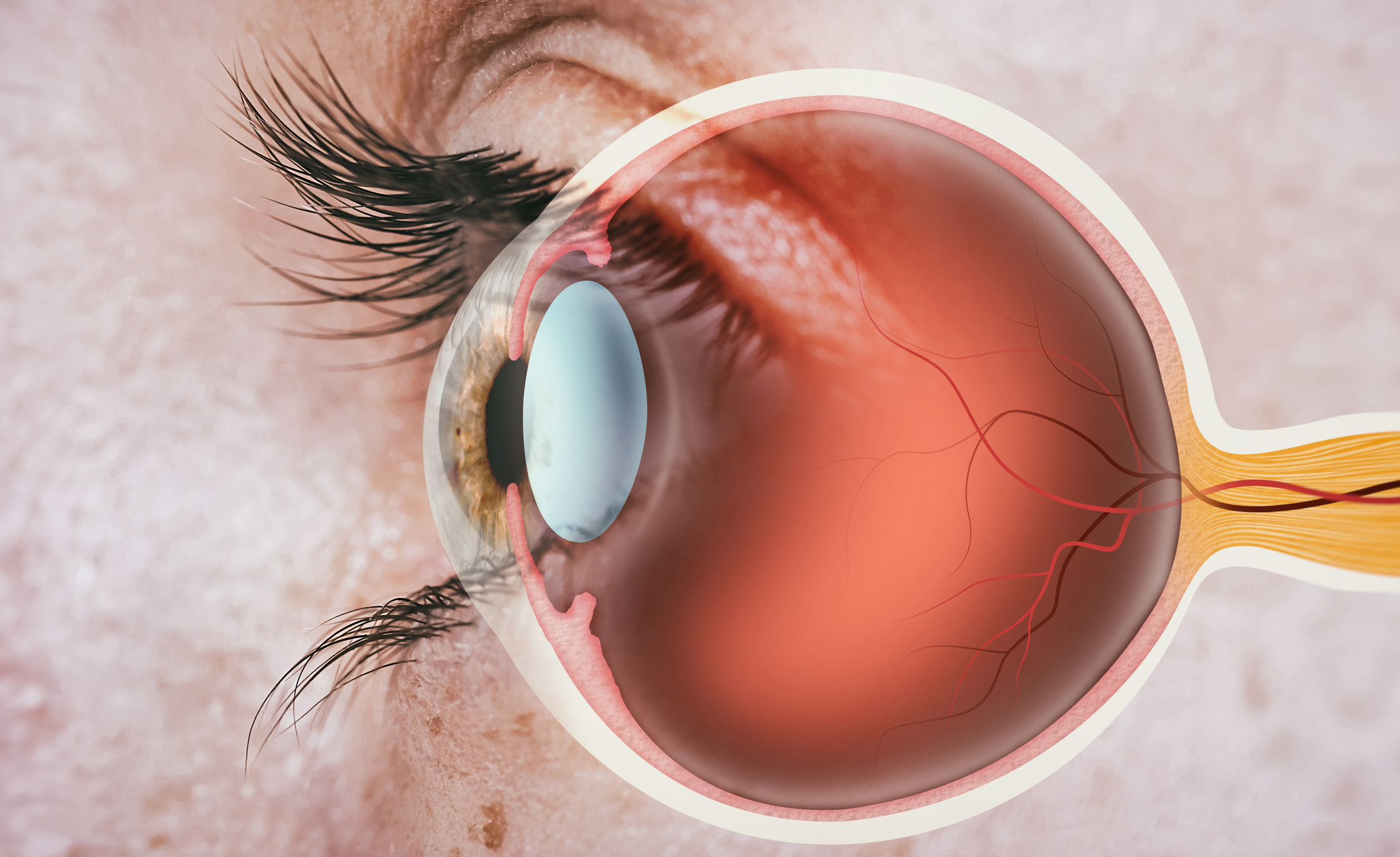
Overview of Retinal Hemorrhage
Retinal hemorrhage refers to bleeding that occurs in the retina, the light-sensitive layer of tissue at the back of the eye. This condition can result from various underlying causes and may lead to visual disturbances or, in severe cases, vision loss.
Symptoms
- Visual Disturbances: Individuals may experience blurred vision, floaters (small specks or particles in the visual field), or sudden vision loss.
- Eye Pain: In some cases, retinal hemorrhage may be associated with eye pain or discomfort.
- Reddish Appearance: The presence of blood in the retina may give the affected eye a reddish appearance.
- Flashes of Light: Some individuals may perceive flashes of light.
Causes
Retinal hemorrhage can be caused by a variety of factors, including:
- Hypertension (High Blood Pressure): Elevated blood pressure can lead to the rupture of small blood vessels in the retina.
- Diabetes: Diabetic retinopathy, a complication of diabetes, can cause damage to the blood vessels in the retina, leading to hemorrhage.
- Age-Related Macular Degeneration (AMD): Abnormal blood vessel growth in the retina associated with AMD can lead to bleeding.
- Retinal Vein Occlusion: Blockage of the retinal veins can result in the backup of blood and subsequent hemorrhage.
- Head Trauma: Injury to the head or eye can cause retinal hemorrhage.
- Blood Disorders: Certain blood disorders or clotting abnormalities can contribute to retinal bleeding.
- Vitreous Hemorrhage: Bleeding into the vitreous humor, the gel-like substance within the eye, can result in secondary retinal hemorrhage.
When to Seek Medical Attention
Prompt medical attention is crucial if you experience symptoms such as:
- Sudden Vision Changes: Any sudden changes in vision, including blurriness, distortion, or loss of vision, should be addressed urgently.
- Floaters and Flashes: The sudden onset of floaters (especially if accompanied by flashes of light) may indicate retinal hemorrhage or other retinal issues.
- Eye Pain: Persistent eye pain or discomfort, especially if accompanied by visual disturbances.
- Head Trauma: If retinal hemorrhage is suspected after head trauma, immediate medical evaluation is necessary.
- Underlying Health Conditions: Individuals with conditions such as hypertension or diabetes should be vigilant for any visual changes and seek medical attention if they occur.
Risk Factors
Several factors increase the risk of developing retinal hemorrhage:
- Hypertension: Uncontrolled high blood pressure is a significant risk factor.
- Diabetes: Individuals with diabetes are at an increased risk of developing diabetic retinopathy and associated retinal hemorrhage.
- Age: Advanced age is associated with an increased risk of age-related macular degeneration and other eye conditions.
- Trauma: Head or eye injuries can lead to retinal hemorrhage.
- Blood Disorders: Certain blood disorders or clotting abnormalities may increase the susceptibility to bleeding in the retina.
- Family History: A family history of retinal issues or systemic conditions affecting the eyes may contribute to the risk.
Regular eye examinations, especially for individuals with underlying health conditions, can aid in the early detection of retinal hemorrhage and other eye problems, allowing for timely intervention and management.
Prevention
While some risk factors for retinal hemorrhage, such as age and family history, may not be modifiable, there are measures individuals can take to potentially reduce the risk and promote overall eye health:
- Control Hypertension: Managing and controlling high blood pressure through lifestyle modifications and, if necessary, medication can help prevent damage to the retinal blood vessels.
- Diabetes Management: Proper management of diabetes, including regular monitoring of blood sugar levels, is crucial for preventing diabetic retinopathy and associated retinal hemorrhage.
- Regular Eye Examinations: Routine eye exams allow for the early detection of conditions that may lead to retinal hemorrhage. Early intervention can prevent or minimize the impact of these conditions.
- Healthy Lifestyle Choices: Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, can contribute to overall eye health.
- Eye Protection: Taking precautions to prevent eye injuries, such as wearing protective eyewear during certain activities, can reduce the risk of trauma-induced retinal hemorrhage.
Diagnosis
- Comprehensive Eye Examination: A comprehensive eye examination by an ophthalmologist will involve a thorough evaluation of the retina using specialized instruments.
- Fundus Photography: Taking photographs of the back of the eye (fundus) can help document the condition of the retina and detect any abnormalities.
- Optical Coherence Tomography (OCT): This imaging technique provides cross-sectional images of the retina, allowing detailed visualization of its layers.
- Fluorescein Angiography: In this test, a special dye is injected into the bloodstream, and images are taken to assess blood flow in the retina.
- Blood Pressure Measurement: Given the association between hypertension and retinal hemorrhage, blood pressure measurement is an important diagnostic step.
Treatment Options
The choice of treatment depends on the underlying cause and severity of retinal hemorrhage:
- Observation: In some cases, particularly if the hemorrhage is minor and not affecting central vision, the approach may be to monitor and observe.
- Vitrectomy: In cases of vitreous hemorrhage, a surgical procedure called vitrectomy may be performed to remove blood from the vitreous humor.
- Laser Photocoagulation: Laser therapy may be used to seal leaking blood vessels in conditions such as diabetic retinopathy.
- Anti-VEGF Injections: Medications that inhibit vascular endothelial growth factor (VEGF), such as ranibizumab or aflibercept, may be injected into the eye to reduce abnormal blood vessel growth.
- Cryotherapy: Freezing treatment (cryotherapy) may be employed to treat abnormal blood vessels in the retina.
Medications
- Anti-VEGF Medications: Injections of anti-VEGF medications can help reduce abnormal blood vessel growth and leakage in conditions like age-related macular degeneration.
- Corticosteroids: In certain cases, corticosteroids may be injected into or around the eye to reduce inflammation and manage retinal hemorrhage.
Follow-Up Care
- Regular Eye Examinations: Continued monitoring through regular eye examinations is crucial to assess the progress of treatment and detect any recurrence or new issues.
- Blood Pressure Management: For individuals with hypertension, ongoing management of blood pressure is essential to prevent further damage to the retinal blood vessels.
- Diabetes Management: Proper control of blood sugar levels is critical for individuals with diabetes to prevent diabetic retinopathy and associated complications.
- Lifestyle Modifications: Adopting and maintaining a healthy lifestyle, including a balanced diet and regular exercise, can contribute to overall eye health.
Demographics More Susceptible
While retinal hemorrhage can occur in individuals of all demographics, certain factors may increase susceptibility:
- Age: The risk of age-related macular degeneration, a condition associated with retinal hemorrhage, increases with age.
- Hypertension: Individuals with high blood pressure are at an elevated risk of retinal hemorrhage.
- Diabetes: Diabetic retinopathy, a common cause of retinal hemorrhage, is more prevalent in individuals with diabetes.
- Genetic Predisposition: A family history of retinal issues or systemic conditions affecting the eyes may contribute to the risk.
- Trauma: Individuals who are at a higher risk of head or eye injuries may have an increased susceptibility to retinal hemorrhage.
Understanding these factors is essential for targeted screening, early detection, and proactive management in at-risk populations. Regular eye check-ups and adherence to preventive measures are key to maintaining eye health and preventing complications associated with retinal hemorrhage.
Conclusion
In conclusion, retinal hemorrhage is a clinical manifestation of various underlying conditions affecting the blood vessels in the retina. Early detection and management of the root cause are crucial for preserving vision and preventing complications. Regular eye examinations, especially for individuals with risk factors such as hypertension or diabetes, play a key role in identifying retinal hemorrhages and initiating appropriate interventions.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Yes, retinal hemorrhages may be associated with systemic health conditions, making it important to address the underlying causes during treatment.
Untreated retinal hemorrhages can lead to permanent vision loss; early detection and appropriate treatment are crucial.
Maintaining a healthy lifestyle, including regular exercise, a balanced diet, and managing systemic health conditions, can contribute to preventing retinal hemorrhages.
Yes, while it can occur in one eye, retinal hemorrhages may affect both eyes, emphasizing the importance of seeking prompt medical attention.
Yes, diabetes can damage blood vessels in the retina, increasing the risk of retinal hemorrhage; regular eye check-ups are essential for individuals with diabetes.
An eye doctor will perform a comprehensive eye exam, including imaging tests like fluorescein angiography or optical coherence tomography.
Yes, uncontrolled high blood pressure is a significant risk factor for retinal hemorrhage; managing blood pressure is crucial.
Yes, trauma to the eye can cause retinal hemorrhage, emphasizing the importance of protective eyewear in certain activities.
Retinal hemorrhages typically do not cause pain, but they can result in sudden vision changes that require immediate attention.
Small retinal hemorrhages may resolve on their own, but prompt medical evaluation is essential for proper management.
news via inbox
Subscribe here to get latest updates !