Solitary Fibrous Tumor (Hemangiopericytoma): An In-Depth Exploration
Introduction
Solitary fibrous tumors (SFTs), including those formerly classified as hemangiopericytomas, are rare neoplasms of mesenchymal origin. These tumors were once considered distinct entities; however, advancements in molecular pathology have unified them under the umbrella of SFTs due to overlapping histological and genetic features. Despite their rarity, SFTs can occur in various anatomical locations, with the orbit being one of the more uncommon sites.
Understanding SFTs is vital due to their variable behavior, ranging from benign, slow-growing masses to aggressive tumors with metastatic potential. This article delves into the etiology, clinical presentation, diagnostic strategies, treatment modalities, and prognosis of SFTs, with a particular focus on their ocular manifestations.
Etiology and Pathogenesis
Genetic and Molecular Basis
The exact pathogenesis of solitary fibrous tumors remains largely speculative, though significant progress has been made in identifying genetic alterations that drive their development. The NAB2-STAT6 gene fusion, resulting from a specific chromosomal translocation (12q13), is a defining feature of SFTs. This fusion gene leads to the constitutive activation of STAT6, a transcription factor that promotes cell proliferation and survival, contributing to tumorigenesis.
While the NAB2-STAT6 fusion is present in most SFTs, it’s important to recognize that these tumors may exhibit a spectrum of genetic changes, reflecting their heterogeneity. For instance, the loss of tumor suppressor genes or mutations in other oncogenes may also play a role in tumor development, particularly in more aggressive or malignant cases.
Histopathological Characteristics
Histologically, SFTs are characterized by a patternless arrangement of spindle-shaped cells set within a dense collagenous stroma. The presence of staghorn-shaped vessels, named for their branching, antler-like appearance, is a hallmark of these tumors. This vascular pattern is reminiscent of hemangiopericytomas, which is why these entities were historically grouped together.
The tumor cells typically express CD34, a marker of vascular endothelial cells, and STAT6, confirming the presence of the NAB2-STAT6 fusion. Other markers like vimentin and BCL-2 are also frequently expressed. Malignant SFTs may display increased cellularity, pleomorphism, high mitotic activity, and areas of necrosis, indicating a more aggressive behavior and worse prognosis.
Clinical Presentation
Ocular and Orbital Manifestations
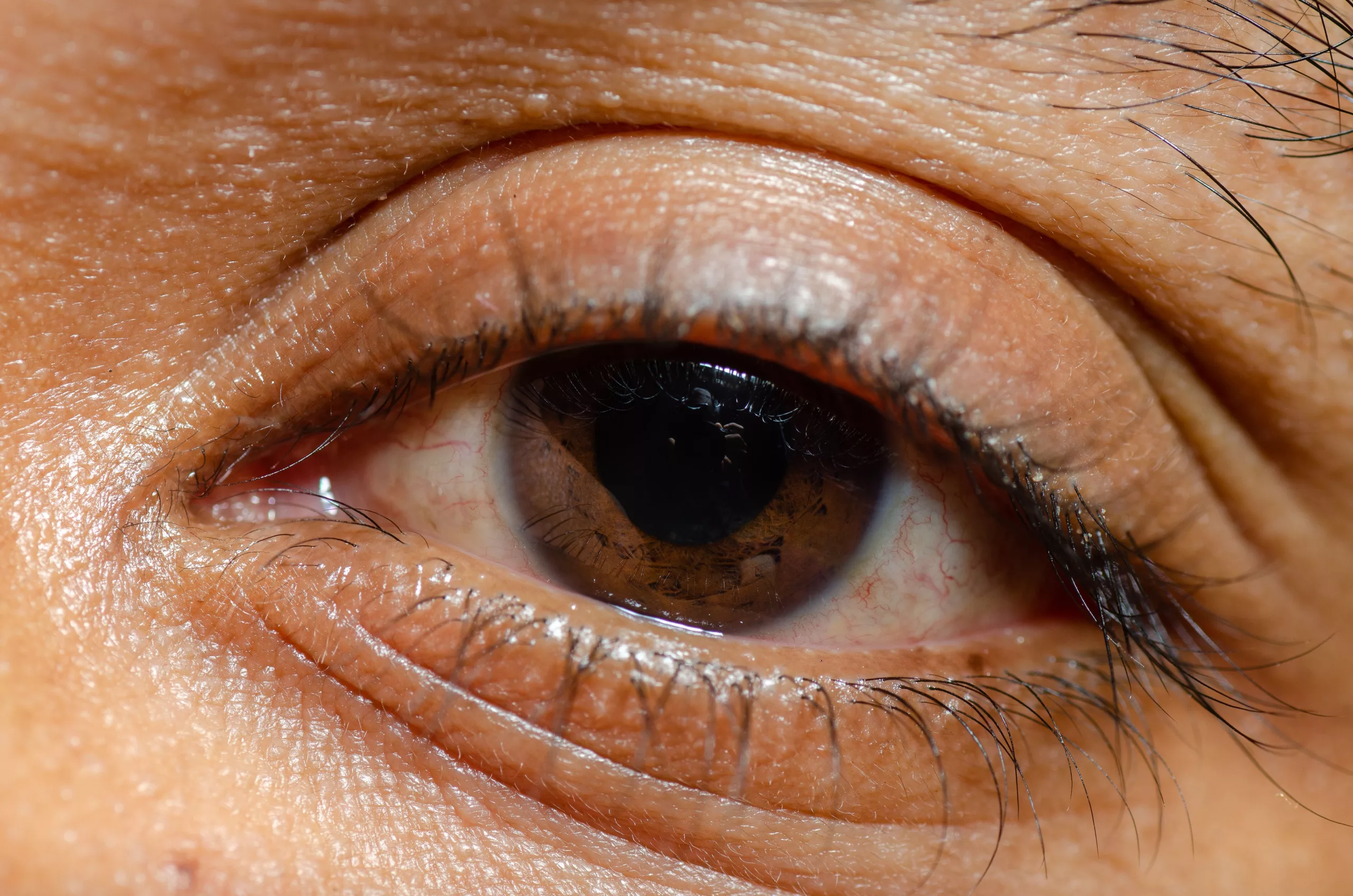
When SFTs occur in the orbit, they typically present as a slowly enlarging mass. The most common symptom is painless proptosis, where the eye is pushed forward due to the growing tumor. This can lead to cosmetic concerns and, in some cases, functional impairments such as restricted eye movement (ophthalmoplegia) or double vision (diplopia).
In some cases, the tumor may compress the optic nerve, leading to visual disturbances, including blurred vision, visual field defects, or even vision loss. Depending on the tumor’s location, patients may also experience discomfort or a palpable mass in the orbital region.
The slow-growing nature of these tumors often leads to delayed presentation, with symptoms developing over months or even years. However, in rare instances, more aggressive SFTs can present with rapid progression and more severe symptoms.
Differential Diagnosis
The presentation of an orbital mass necessitates a broad differential diagnosis. SFTs must be distinguished from other spindle cell neoplasms and vascular tumors, such as:
- Meningiomas: These tumors also present with proptosis and may exhibit calcifications. However, meningiomas are typically dural-based and may encase the optic nerve.
- Schwannomas: These nerve sheath tumors may present similarly but are distinguished by their origin from cranial or peripheral nerves.
- Hemangiomas: These benign vascular tumors are more common in children and often present with a different vascular pattern on imaging.
- Orbital Lymphomas: Typically present in older adults and are associated with systemic signs or B symptoms (fever, night sweats, weight loss).
Diagnosis
Imaging Studies
Imaging plays a crucial role in the diagnosis and management of SFTs. The tumor’s radiological appearance, combined with clinical findings, can provide valuable information regarding its nature and extent.
- Magnetic Resonance Imaging (MRI): MRI is the gold standard for evaluating SFTs, particularly in the orbit where detail and soft tissue contrast are critical. On T1-weighted images, SFTs often appear isointense to muscle, while T2-weighted images may show a variable signal intensity, reflecting the tumor’s fibrous content. Contrast-enhanced MRI typically reveals heterogeneous enhancement, which helps delineate the tumor from surrounding tissues.
- Computed Tomography (CT) Scan: CT imaging is particularly useful in assessing bony involvement, which is critical when SFTs arise in the orbit. CT scans may reveal a well-defined, lobulated mass with variable enhancement. Calcifications, though uncommon, can be detected on CT, and the scan may also highlight any bony erosion or remodeling caused by the tumor.
Histopathological Examination
A definitive diagnosis of SFT is established through histopathological examination, which involves both microscopic analysis and immunohistochemical staining.
- Microscopy: The tumor is examined under the microscope to identify the characteristic spindle-shaped cells and the patternless architecture within a collagenous matrix. The staghorn vessel pattern is another key diagnostic feature.
- Immunohistochemistry: The use of immunohistochemical stains is essential for distinguishing SFTs from other spindle cell tumors. The presence of CD34 and nuclear STAT6 positivity, along with the absence of markers for other neoplasms (e.g., S-100 for schwannomas), helps confirm the diagnosis.
- Genetic Testing: In challenging cases, genetic testing to identify the NAB2-STAT6 fusion gene can provide additional confirmation, particularly in tumors with atypical histological features.
Differential Diagnosis
Given the diverse range of orbital tumors, distinguishing SFTs from other entities is crucial. In addition to the tumors mentioned previously, other differential considerations include:
- Fibrous Histiocytoma: A benign spindle cell tumor that can mimic SFTs but typically lacks the staghorn vessels and CD34 positivity.
- Synovial Sarcoma: A malignant spindle cell tumor that can present similarly but often exhibits distinct histological features and different genetic markers.
- Leiomyoma: A smooth muscle tumor that may appear similar on imaging but is distinguished by smooth muscle markers like desmin and actin.
Treatment
Surgical Management
The cornerstone of SFT treatment is complete surgical excision. The goal is to achieve clear margins to reduce the risk of recurrence, which can be challenging, especially in anatomically complex regions like the orbit.
- Surgical Techniques: The choice of surgical approach depends on the tumor’s size, location, and the structures involved. In the orbit, an anterior orbitotomy or lateral orbitotomy is commonly performed to access the tumor. In cases where the tumor is adjacent to critical structures like the optic nerve or extraocular muscles, meticulous dissection is required to avoid damaging these structures.
- Intraoperative Considerations: Surgeons must carefully plan the resection to achieve complete removal while preserving function. In some cases, intraoperative imaging or navigation tools may be used to ensure that the tumor is fully excised.
Adjuvant Therapy
- Radiotherapy: While surgery is the primary treatment, radiotherapy may be considered in cases where complete excision is not possible, or where the tumor exhibits malignant features. Radiotherapy can help control local disease and reduce the risk of recurrence. The decision to use radiotherapy is typically based on the tumor’s histological grade, margin status, and patient factors.
- Chemotherapy: Chemotherapy is generally reserved for cases of metastatic or unresectable SFTs. However, its role is limited, and there is no established standard regimen. Chemotherapeutic agents may be selected based on the tumor’s specific characteristics, but the overall response rates are typically low.
Emerging Therapies
Research into the molecular and genetic underpinnings of SFTs has opened the door to potential targeted therapies. For example, inhibitors targeting the NAB2-STAT6 fusion gene or related pathways may offer new treatment options, particularly for aggressive or recurrent tumors. Clinical trials are ongoing to evaluate the efficacy of these targeted approaches.
Prognosis
Factors Influencing Prognosis
The prognosis of solitary fibrous tumors varies widely and is influenced by several factors:
- Tumor Size and Location: Larger tumors or those located in critical areas (such as near the optic nerve) may be more challenging to resect completely, increasing the risk of recurrence.
- Histopathological Features: Tumors with malignant features—such as high mitotic activity, cellular atypia, and necrosis—tend to have a worse prognosis. These features are associated with a higher likelihood of local recurrence and distant metastasis.
- Surgical Margins: The completeness of surgical resection is a key prognostic factor. Tumors that are completely excised with clear margins generally have a better outcome. Incomplete resection increases the risk of recurrence, which can occur many years after the initial surgery.
Recurrence and Long-Term Follow-Up
Recurrence is a significant concern with SFTs, especially those with malignant features. Recurrences can occur many years after the initial treatment, necessitating long-term follow-up. Patients should undergo regular clinical and imaging evaluations to monitor for signs of recurrence.
The follow-up schedule may vary depending on the individual case but typically involves annual imaging for at least the first five years after surgery, with continued surveillance beyond that period if risk factors for recurrence are present.
Metastasis and Survival
While the majority of SFTs are benign, a small percentage can metastasize to distant organs, including the lungs, liver, and bones. Metastatic disease significantly worsens the prognosis, and survival rates decrease accordingly. The five-year survival rate for patients with metastatic SFTs is significantly lower than for those with localized disease.
Conclusion
Solitary fibrous tumors (hemangiopericytomas) represent a complex and heterogeneous group of neoplasms with a wide spectrum of clinical behavior. Early recognition, accurate diagnosis, and appropriate treatment are essential for achieving the best possible outcomes. While most SFTs are benign, their potential for malignant transformation and recurrence necessitates careful long-term follow-up.
Advances in genetic and molecular research are providing new insights into the pathogenesis of SFTs, which may lead to the development of more targeted therapies in the future. These therapies could improve outcomes for patients with aggressive or recurrent tumors, offering hope for better management of this challenging condition.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Solitary fibrous tumors (SFTs) and hemangiopericytomas were once considered separate entities, but they are now classified under the same category due to their similar histological and genetic features. The main difference historically was the vascular pattern, with hemangiopericytomas being more vascular. However, both tumors are now recognized as part of the SFT spectrum.
Yes, solitary fibrous tumors can recur even after complete surgical removal, especially if the tumor has malignant features. Long-term follow-up with regular imaging is crucial to monitor for recurrence.
Currently, there are no known lifestyle changes that can prevent the development of solitary fibrous tumors. These tumors are generally sporadic and not linked to specific environmental or lifestyle factors.
Genetic testing, particularly for the NAB2-STAT6 gene fusion, can be helpful in confirming the diagnosis of SFT, especially in atypical cases. However, it is not always necessary if the tumor’s histological and immunohistochemical features are clear.
Solitary fibrous tumors can occur at any age, but they most commonly present in middle-aged adults. However, cases have been reported in both younger and older patients.
While most solitary fibrous tumors are benign, some can metastasize to distant organs such as the lungs, liver, or bones. This is more common in tumors with malignant features.
Solitary fibrous tumors are distinct in their histological appearance, characterized by spindle cells in a collagenous matrix with a patternless growth and staghorn-shaped vessels. Their diagnosis often requires immunohistochemical staining, which distinguishes them from other orbital tumors like meningiomas, schwannomas, and hemangiomas.
Solitary fibrous tumors in the orbit can cause vision loss if they compress the optic nerve. If diagnosed and treated early, vision loss may be reversible, but permanent damage can occur if the tumor is not promptly addressed.
Surgery to remove an orbital SFT carries risks such as damage to the optic nerve, extraocular muscles, or other critical structures in the orbit. There is also a risk of incomplete removal, leading to recurrence. However, with careful surgical planning, these risks can be minimized.
Solitary fibrous tumors are generally not associated with hereditary syndromes and are considered sporadic tumors. There is no evidence to suggest a familial pattern or genetic predisposition.
news via inbox
Subscribe here to get latest updates !