Understanding Anterior Uveitis
Introduction
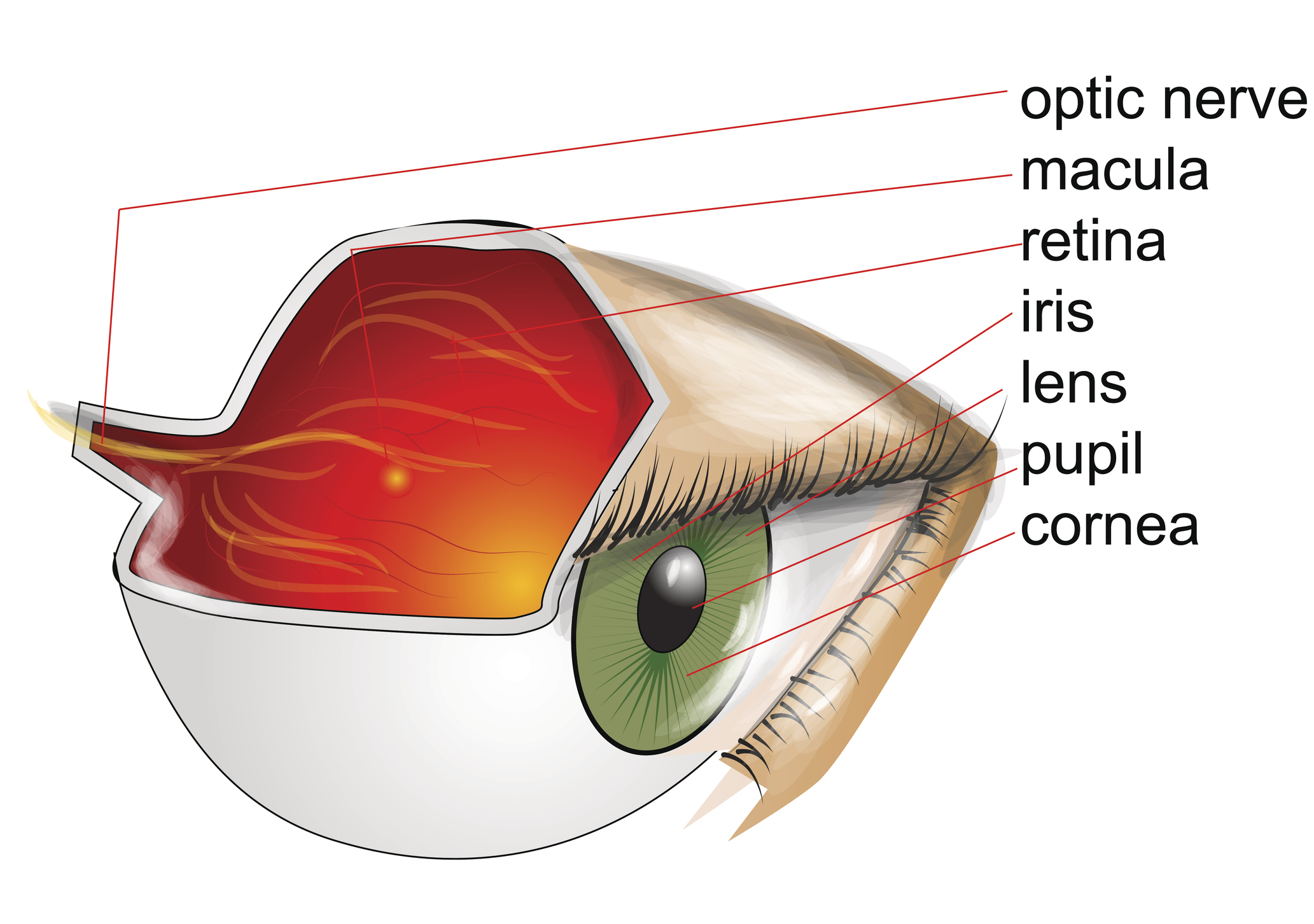
Anterior uveitis, also known as iritis, is a form of uveitis that affects the front portion of the eye. This condition involves inflammation of the uvea, the middle layer of the eye, which includes the iris (colored part of the eye) and the ciliary body. Anterior uveitis can cause discomfort, vision changes, and, if left untreated, potentially serious complications. Here, we’ll explore the symptoms, causes, diagnosis, and treatment options for anterior uveitis.
Symptoms
- Eye Pain: Anterior uveitis often presents with moderate to severe eye pain, which may be described as a dull ache or a sharp, stabbing sensation. The pain is typically worsened by eye movement and can vary in intensity.
- Redness: The affected eye may appear red or bloodshot due to the inflammation of the iris and surrounding blood vessels. This redness is often more pronounced near the cornea.
- Photophobia: Patients with anterior uveitis are often sensitive to light (photophobia), experiencing discomfort or pain when exposed to bright lights or sunlight. They may squint or shield their eyes in response to light.
- Blurred Vision: Blurred vision is common in anterior uveitis and can result from inflammation-induced changes in the shape of the iris or from the presence of inflammatory cells in the aqueous humor, the fluid that fills the front of the eye.
- Tearing: Excessive tearing or watery eyes can occur as a result of the eye’s inflammatory response to the uveitis. This symptom is often accompanied by irritation and discomfort.
- Small Pupil: In some cases, the pupil of the affected eye may constrict (miosis) due to inflammation of the iris muscles, leading to a smaller-than-normal pupil size.
Causes
Anterior uveitis can have various causes, including:
- Autoimmune Disorders: Conditions such as rheumatoid arthritis, ankylosing spondylitis, and inflammatory bowel disease are associated with anterior uveitis. In these cases, the body’s immune system mistakenly attacks the tissues of the eye, leading to inflammation.
- Infections: Bacterial, viral, fungal, or parasitic infections can trigger anterior uveitis. Common infectious causes include herpes simplex virus, varicella-zoster virus, tuberculosis, syphilis, and toxoplasmosis.
- Trauma: Eye injuries or trauma, such as a blow to the eye or a penetrating injury, can lead to inflammation of the iris and surrounding tissues.
- Idiopathic: In many cases, the exact cause of anterior uveitis remains unknown (idiopathic). It may occur spontaneously or be triggered by unknown factors.
Diagnosis
Diagnosing anterior uveitis typically involves a comprehensive eye examination and evaluation of the patient’s medical history. Key steps in the diagnostic process include:
- Medical History: The healthcare provider will inquire about the patient’s symptoms, medical history, recent illnesses, past eye injuries or surgeries, and any underlying medical conditions or autoimmune disorders.
- Physical Examination: A thorough eye examination will be performed to assess the external and internal structures of the eye. This may include visual acuity testing, assessment of eye pressure, examination of the eyelids, conjunctiva, and cornea, and evaluation of the pupil size and reaction to light.
- Slit-Lamp Biomicroscopy: A slit-lamp examination allows for detailed visualization of the anterior segment of the eye, including the iris, anterior chamber, and lens. Using a specialized microscope called a slit lamp, the healthcare provider can identify signs of inflammation, such as cells or flare in the anterior chamber and inflammation of the iris (iritis).
- Dilation: Dilation of the pupil with dilating eye drops facilitates examination of the posterior segment of the eye, including the retina and optic nerve. This helps rule out associated complications and determine the extent of inflammation.
- Laboratory Tests: Depending on the suspected cause of anterior uveitis, additional laboratory tests may be ordered to detect infectious agents (e.g., blood tests for viruses or serological tests for syphilis), assess inflammatory markers (e.g., erythrocyte sedimentation rate, C-reactive protein), or screen for underlying systemic diseases (e.g., autoimmune antibodies).
Treatment of Anterior Uveitis
Treatment for anterior uveitis aims to alleviate inflammation, relieve symptoms, prevent complications, and preserve vision. The approach to treatment may vary depending on the severity of the condition, underlying causes, and individual patient factors. Here’s a detailed overview of the treatment modalities commonly used for anterior uveitis:
- Topical Corticosteroids:
- Corticosteroid eye drops are the primary treatment for anterior uveitis. These medications work by reducing inflammation in the eye. Commonly prescribed corticosteroid eye drops include prednisolone acetate, dexamethasone, and fluorometholone.
- Treatment typically begins with frequent administration of corticosteroid eye drops, often every 1 to 2 hours initially, then gradually tapered as inflammation improves. The dosage and frequency of eye drops may be adjusted based on the response to treatment and the severity of inflammation.
- It’s essential to follow the prescribed regimen carefully and continue using the medication as directed by your healthcare provider, even if symptoms improve, to prevent recurrence of inflammation.
- Cycloplegic Agents:
- Cycloplegic or mydriatic eye drops, such as cyclopentolate or atropine, are often used as adjunctive therapy in the treatment of anterior uveitis. These medications help dilate the pupil and relax the muscles of the iris, reducing pain and preventing the formation of posterior synechiae (adhesions between the iris and lens).
- Cycloplegic agents may be particularly beneficial in cases of severe uveitis or when there is significant pain or photophobia.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- NSAID eye drops, such as ketorolac or bromfenac, may be used in combination with corticosteroid eye drops to provide additional anti-inflammatory and analgesic effects. NSAIDs help reduce inflammation and relieve pain associated with anterior uveitis.
- Combination therapy with corticosteroids and NSAIDs may be especially useful in cases of moderate to severe inflammation or when corticosteroids alone are insufficient to control symptoms.
- Systemic Treatment:
- In cases of severe anterior uveitis, recurrent uveitis, or when there is associated systemic disease, systemic corticosteroids or immunosuppressive medications may be prescribed. These medications are taken orally or administered intravenously and work to suppress the immune system and reduce inflammation throughout the body.
- Systemic treatment may be necessary to achieve adequate control of inflammation and prevent complications, but it also carries potential side effects and requires close monitoring by a healthcare provider.
- Monitoring and Follow-up:
-
- Regular follow-up appointments with an ophthalmologist are crucial for monitoring the response to treatment, assessing for any complications, and adjusting therapy as needed. During follow-up visits, the ophthalmologist will evaluate visual acuity, intraocular pressure, signs of inflammation, and any changes in eye health.
- Long-term management may involve tapering corticosteroid eye drops gradually, transitioning to less frequent dosing, or switching to alternative medications as inflammation resolves.
When to Consult a Doctor
It’s important to consult an eye doctor promptly if you experience symptoms suggestive of anterior uveitis, such as:
- Moderate to severe eye pain
- Redness or irritation of the eye
- Sensitivity to light (photophobia)
- Blurred vision
- Excessive tearing
- Floaters or spots in your vision
Additionally, individuals with known risk factors for uveitis, such as autoimmune diseases, a history of eye trauma, or a family history of uveitis, should undergo regular eye examinations to monitor for signs of inflammation and promptly address any issues that arise.
If you are unsure whether your symptoms warrant medical attention, it’s best to err on the side of caution and seek evaluation by a healthcare professional. Early diagnosis and treatment of anterior uveitis are essential for preventing complications and preserving vision. Delaying treatment may lead to worsening inflammation, increased risk of complications, and permanent damage to the eye.
Conclusion
Anterior uveitis is a potentially serious eye condition characterized by inflammation of the iris and surrounding tissues. Prompt diagnosis and appropriate treatment are essential for minimizing discomfort, preserving vision, and preventing complications. Individuals experiencing symptoms of anterior uveitis should seek evaluation by an eye care professional for proper diagnosis and management tailored to their specific needs.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Some individuals may explore complementary therapies such as acupuncture, dietary supplements, or herbal remedies for symptom relief. However, it’s essential to consult with a healthcare professional before trying any alternative treatments, as they may interact with conventional medications or have unknown side effects.
Stress can potentially exacerbate symptoms in individuals with autoimmune conditions predisposing them to anterior uveitis. Managing stress through relaxation techniques, mindfulness, and adequate sleep may help reduce the frequency or severity of flare-ups.
While there may be genetic predispositions to autoimmune conditions associated with anterior uveitis, the condition itself is not directly hereditary. However, family history of autoimmune diseases may increase the risk of developing uveitis.
It’s important to follow your doctor’s recommendations regarding driving while experiencing symptoms of anterior uveitis. If your vision is significantly impaired or if you are taking medications that affect your ability to drive safely, it may be advisable to refrain from driving until your condition improves.
Anterior uveitis can occur in individuals of any age, but it is more commonly diagnosed in adults aged 20 to 50 years. It may also be more prevalent in individuals with certain autoimmune conditions or genetic predispositions.
While lifestyle changes alone cannot prevent anterior uveitis, maintaining overall health through a balanced diet, regular exercise, and stress management may support immune function and reduce the risk of flare-ups in individuals predisposed to uveitis.
While anterior uveitis can be effectively managed with treatment, it may recur intermittently, especially in cases associated with underlying systemic conditions. With proper management, most individuals can achieve symptom relief and prevent complications.
Untreated anterior uveitis can lead to complications such as glaucoma, cataracts, and permanent vision loss. It’s essential to seek prompt medical attention to prevent these complications.
It’s best to avoid wearing contact lenses during an episode of anterior uveitis, as they can exacerbate discomfort and potentially increase the risk of complications. Consult your eye doctor for personalized advice.
No, anterior uveitis is not contagious. It is typically caused by underlying autoimmune conditions, infections, or trauma, rather than by person-to-person transmission.
news via inbox
Subscribe here to get latest updates !