Unveiling Hollenhorst Plaques: Causes, Symptoms
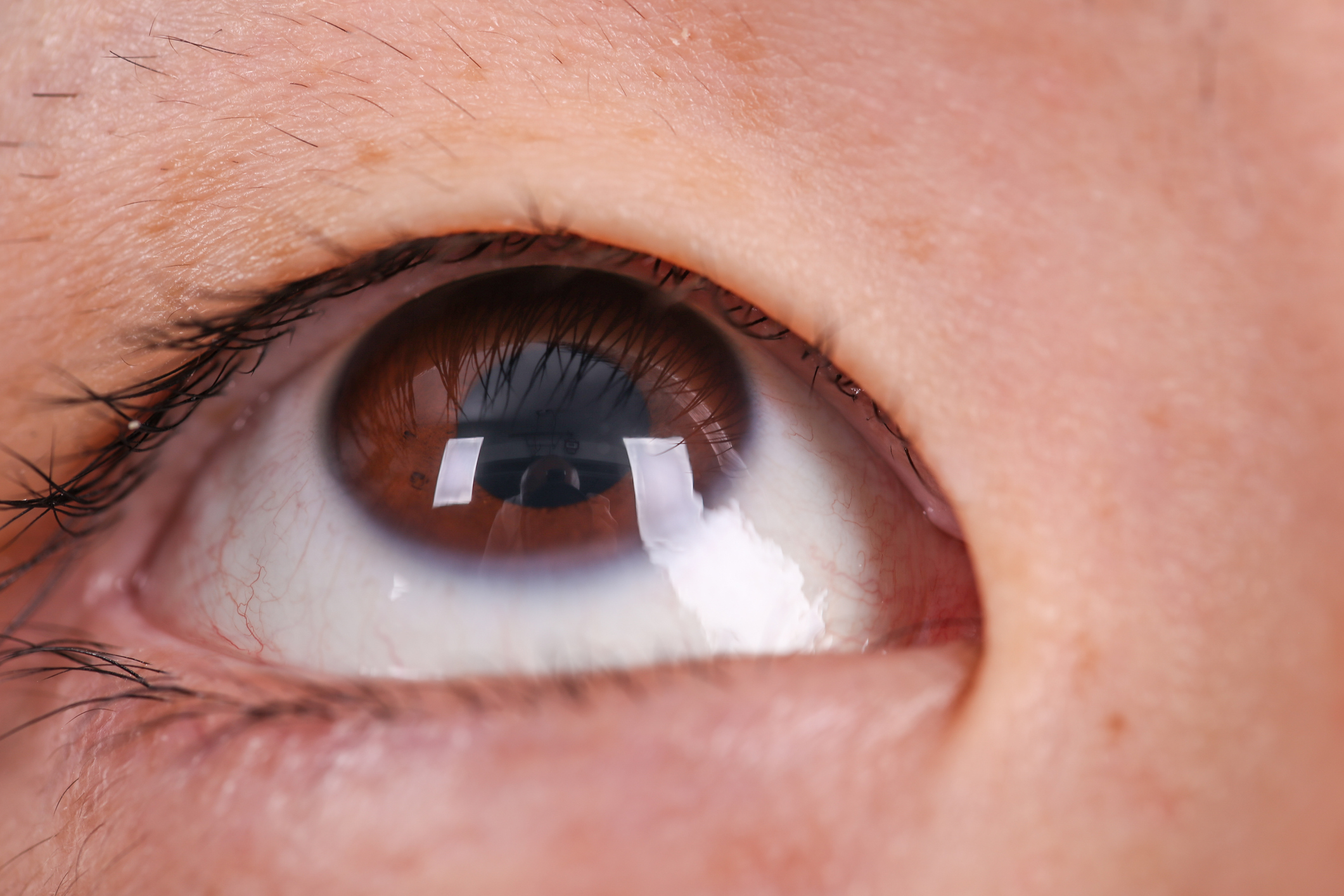
Hollenhorst plaques are cholesterol emboli that can lodge in the small blood vessels of the eye, posing a risk of retinal damage. This article provides a detailed and empathetic guide to Hollenhorst plaques, covering their causes, symptoms, when to seek medical attention, diagnosis, treatment options, and preventive measures.
Overview of Hollenhorst Plaques
Hollenhorst plaques are small cholesterol emboli that can lodge in the small blood vessels of the eye, specifically in the retina. These emboli are composed of cholesterol crystals and can lead to a disruption in blood flow, potentially causing damage to the retina and affecting vision. Hollenhorst plaques are named after Dr. Carl Hollenhorst, who first described them in 1958.
Causes
The primary cause of Hollenhorst plaques is atherosclerosis, a condition characterized by the build-up of cholesterol and other substances in the arteries. As atherosclerosis progresses, plaques can form in the blood vessels throughout the body, including those in the eye. When a plaque breaks loose, it can travel through the bloodstream and eventually become lodged in the smaller vessels of the retina, causing a blockage.
Symptoms
- Visual Disturbances: The most common symptom associated with Hollenhorst plaques is sudden visual disturbances. Patients may experience sudden blurry vision, partial vision loss, or see floating spots or lines in their field of vision.
- Painless Nature: Hollenhorst plaque-induced symptoms are typically painless. Patients may not experience any discomfort or eye pain, but the sudden onset of visual changes should prompt further investigation.
- Unilateral Affection: Hollenhorst plaques often affect only one eye. If both eyes are affected, it usually happens at different times.
When to Seek Medical Attention
Prompt medical attention is crucial if any of the following symptoms occur:
- Sudden Vision Changes: Any sudden changes in vision, especially if associated with floating spots or lines, should be evaluated by an eye care professional.
- Partial or Complete Vision Loss: If there is partial or complete vision loss, it is considered a medical emergency, and immediate attention is required.
- Painless Vision Disturbances: Even if the visual disturbances are painless, they should not be ignored. Seeking medical advice promptly can help determine the cause and prevent potential complications.
- Risk Factors: Individuals with known risk factors for atherosclerosis, such as hypertension, diabetes, or a history of cardiovascular disease, should be vigilant about any changes in vision and seek medical attention if necessary.
- Regular Eye Exams: Routine eye examinations are essential, especially for those with risk factors. Regular check-ups can help detect and manage conditions like atherosclerosis before they lead to serious complications such as Hollenhorst plaques.
In summary, Hollenhorst plaques, caused by cholesterol emboli lodging in the retinal blood vessels, can result in sudden visual disturbances. Understanding the symptoms and knowing when to seek medical attention is crucial for timely diagnosis and intervention, potentially preventing further damage to the retina and preserving vision.
Diagnosis
- Comprehensive Eye Examination: An eye care professional will conduct a thorough examination, including a dilated eye exam, to assess the retina and look for signs of Hollenhorst plaques.
- Fluorescein Angiography: This diagnostic procedure involves injecting a special dye into the bloodstream and capturing images as it circulates through the retinal blood vessels. It helps identify blockages caused by Hollenhorst plaques.
- Optical Coherence Tomography (OCT): This imaging test uses light waves to create detailed cross-sectional images of the retina, providing a closer look at the affected areas and aiding in the diagnosis.
- Blood Tests: Laboratory tests, including lipid profiles, may be performed to assess cholesterol levels and identify potential underlying causes such as hyperlipidemia.
Treatment Options
- Observation: In some cases, especially if the Hollenhorst plaque is small and not causing significant vision problems, a “watch and wait” approach may be adopted. Regular monitoring and lifestyle modifications may be recommended.
- Antiplatelet Medications: Medications like aspirin may be prescribed to prevent the formation of blood clots, reducing the risk of further emboli.
- Cholesterol-Lowering Medications: Statins and other cholesterol-lowering medications may be prescribed to manage underlying atherosclerosis and prevent the recurrence of Hollenhorst plaques.
- Lifestyle Modifications: Adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, and smoking cessation, can contribute to overall cardiovascular health and reduce the risk of atherosclerosis-related conditions.
- Surgical Intervention: In rare cases where the blockage is severe or vision is significantly compromised, surgical procedures such as retinal laser therapy or vitrectomy may be considered.
Preventive Measures
- Manage Cardiovascular Risk Factors: Control factors contributing to atherosclerosis, such as hypertension, diabetes, and high cholesterol, through lifestyle modifications and medication as prescribed by healthcare professionals.
- Regular Exercise: Engage in regular physical activity to promote cardiovascular health and reduce the risk of atherosclerosis.
- Healthy Diet: Adopt a diet rich in fruits, vegetables, whole grains, and lean proteins while minimizing saturated and trans fats to maintain optimal cholesterol levels.
- Regular Eye Check-ups: Routine eye examinations are essential, especially for individuals with cardiovascular risk factors. Early detection and management of conditions like atherosclerosis can prevent complications like Hollenhorst plaques.
Demographics More Susceptible
- Age: The risk of atherosclerosis and related conditions, including Hollenhorst plaques, increases with age.
- Cardiovascular Risk Factors: Individuals with hypertension, diabetes, high cholesterol, smoking habits, and a history of cardiovascular disease are more susceptible.
- Genetic Predisposition: A family history of cardiovascular diseases may contribute to an increased susceptibility.
- Gender: Men are generally at a higher risk compared to women, particularly as they age.
Understanding the diagnosis, treatment options, preventive measures, and demographics more susceptible to Hollenhorst plaques is crucial for both healthcare professionals and individuals to manage and mitigate the impact of this condition on vision and overall health.
Conclusion
Understanding the causes, recognizing potential symptoms, and adopting management strategies are key components in addressing Hollenhorst plaques. By prioritizing vascular health and seeking timely medical attention, individuals can actively contribute to maintaining optimal vision and overall well-being.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Adopting a heart-healthy diet, low in saturated fats and cholesterol, can contribute to vascular health and help prevent conditions associated with Hollenhorst plaques.
With appropriate management and addressing underlying vascular issues, individuals with Hollenhorst plaques can lead a normal life. Regular medical follow-ups are essential.
While Hollenhorst plaques themselves may not be reversed, addressing underlying vascular issues through medication and lifestyle changes can contribute to overall vascular health.
Hollenhorst plaques may indicate underlying vascular issues, such as atherosclerosis. Addressing these issues is crucial to prevent further complications.
Risk factors for Hollenhorst plaques are often associated with atherosclerosis, including age, high blood pressure, high cholesterol, and smoking.
Yes, Hollenhorst plaques can be detected during a comprehensive eye examination, particularly if they are impacting the blood vessels in the retina.
Hollenhorst plaques themselves do not typically require surgical removal. Management focuses on addressing underlying vascular issues through medication and lifestyle changes.
While Hollenhorst plaques can occur in either eye, their impact is often observed in one eye. It’s essential to seek prompt medical attention if any visual changes occur.
Not all individuals with Hollenhorst plaques experience noticeable symptoms. Regular eye examinations are essential for detecting these plaques and assessing their potential impact on vision.
The impact of Hollenhorst plaques on vision can vary. Prompt medical attention and addressing underlying vascular issues are crucial for minimizing the risk of permanent vision loss.
news via inbox
Subscribe here to get latest updates !