Comprehensive Insights on Scleritis
Introduction
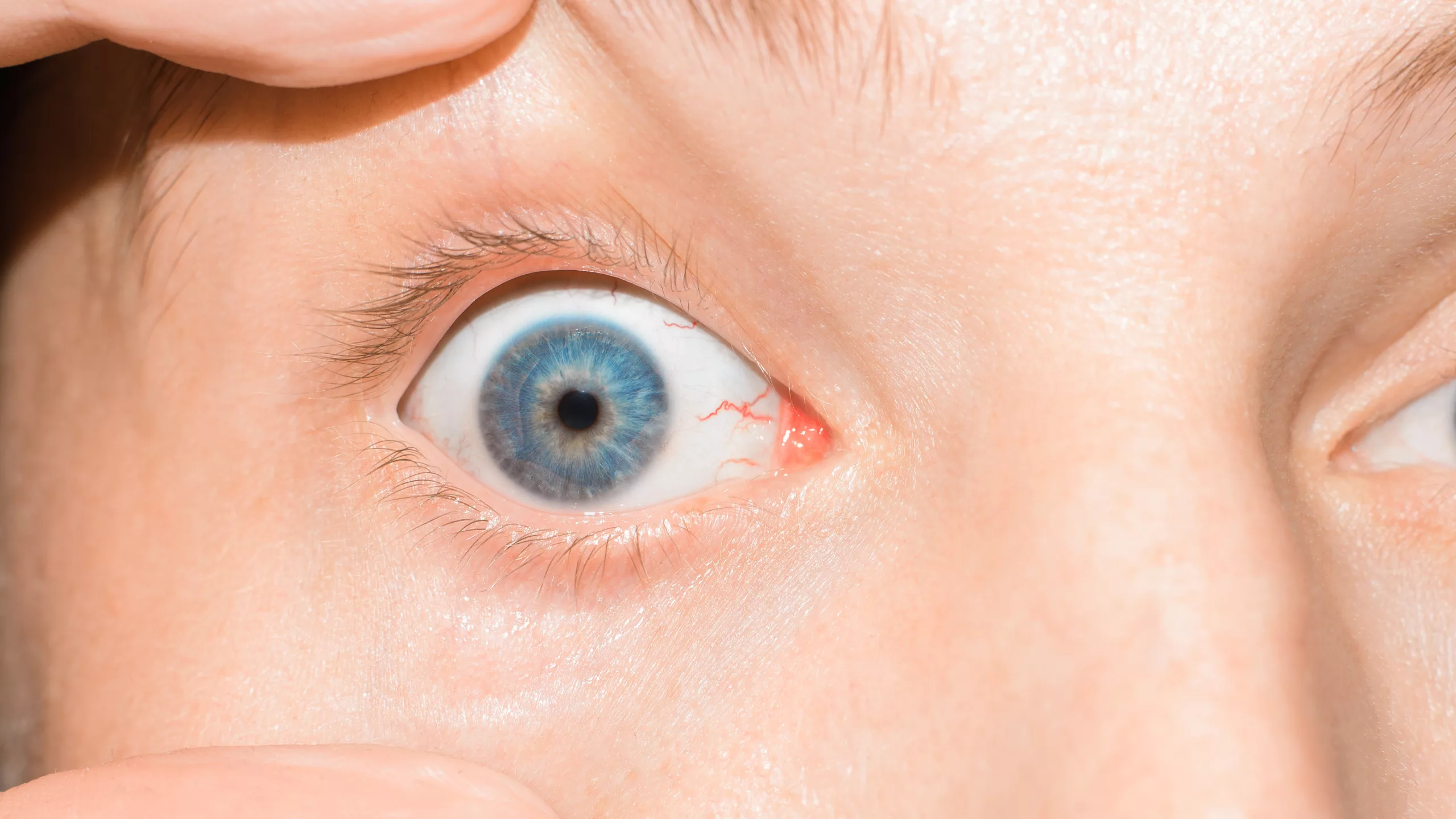
Scleritis is a severe, potentially vision-threatening condition characterized by inflammation of the sclera, the white outer coating of the eye. Although relatively rare, scleritis can cause significant discomfort and complications if not treated promptly. This article provides an in-depth exploration of scleritis, including its symptoms, causes, types, diagnosis, treatment options, and preventive measures.
What is Scleritis?
The sclera is the protective outer layer of the eye, maintaining its shape and safeguarding the inner components. It is composed of dense connective tissue and provides a sturdy framework that supports the eye’s structure. Scleritis occurs when this layer becomes inflamed, leading to redness, pain, and, in severe cases, vision loss. Unlike more common conditions such as conjunctivitis, scleritis is often associated with underlying systemic diseases, making it critical to diagnose and manage effectively.
Anatomy of the Sclera
The sclera, also known as the “white of the eye,” is about 0.3 to 1.0 millimeters thick and covers approximately five-sixths of the eye’s surface. It is composed of collagen and elastic fibers, giving it both strength and flexibility. The sclera provides attachment points for the extraocular muscles, which control eye movement. The sclera’s primary function is to protect the internal structures of the eye from injury and to maintain the shape of the eye.
Symptoms of Scleritis
Recognizing the symptoms of scleritis early can help in seeking timely medical intervention. The common symptoms include:
- Severe Eye Pain: Unlike the discomfort of conjunctivitis, the pain associated with scleritis is often deep, severe, and can radiate to the face and jaw. The pain tends to worsen with eye movement or during the night and can be severe enough to interfere with sleep and daily activities.
- Redness: The affected eye may appear red due to the inflamed blood vessels in the sclera. This redness is more intense and localized than the redness seen in conjunctivitis, often involving a significant portion of the sclera.
- Visual Disturbances: Blurred vision or decreased vision may occur if the inflammation affects deeper structures of the eye, such as the cornea, retina, or optic nerve. Double vision or seeing “halos” around lights may also be reported.
- Sensitivity to Light: Photophobia, or sensitivity to light, is a common symptom and can cause significant discomfort in bright environments, necessitating the use of sunglasses or dimming lights.
- Tearing: Excessive tearing or watery eyes may accompany other symptoms, as the eye attempts to lubricate and soothe the irritated sclera.
- Tenderness: The sclera may be tender to touch, and applying pressure to the eye can exacerbate the pain.
- Reduced Eye Movement: In severe cases, the inflammation may restrict eye movement, causing additional pain when attempting to move the eyes.
Causes and Risk Factors
Scleritis is often associated with autoimmune disorders, where the body’s immune system mistakenly attacks its own tissues. Common underlying conditions include:
- Rheumatoid Arthritis: A significant number of scleritis cases are linked to rheumatoid arthritis, an autoimmune condition that causes chronic inflammation of joints and other tissues. The inflammation in rheumatoid arthritis can extend to the sclera, leading to scleritis.
- Systemic Lupus Erythematosus (SLE): Lupus can cause widespread inflammation, including in the sclera. It is characterized by the body’s immune system attacking healthy tissues, leading to various systemic complications, including scleritis.
- Ankylosing Spondylitis: This form of arthritis primarily affects the spine but can also lead to scleritis. It causes inflammation of the vertebrae, which can spread to other parts of the body, including the eyes.
- Granulomatosis with Polyangiitis (GPA): Formerly known as Wegener’s granulomatosis, GPA is an autoimmune disease that causes inflammation of the blood vessels, including those in the eyes, leading to scleritis.
- Infections: Although less common, certain bacterial, fungal, or viral infections can trigger scleritis. These infections can directly invade the sclera or spread from adjacent tissues. For example, herpes zoster (shingles) can cause scleritis if it involves the ophthalmic nerve.
- Surgery or Trauma: Previous eye surgery or trauma can increase the risk of developing scleritis, particularly if there is residual inflammation or scarring. This can be due to direct injury to the sclera or post-surgical complications.
Additional Risk Factors
- Gender: Women are more commonly affected by scleritis, likely due to the higher prevalence of autoimmune diseases in females.
- Age: Scleritis is most frequently diagnosed in adults between the ages of 30 and 60.
- Genetics: A family history of autoimmune diseases may increase the risk of developing scleritis.
- Environmental Factors: Exposure to certain environmental factors, such as infections or pollutants, may trigger scleritis in susceptible individuals.
Types of Scleritis
Scleritis is categorized based on the location and severity of the inflammation:
- Anterior Scleritis: The most common form, affecting the front portion of the sclera. It is further divided into:
- Diffuse Anterior Scleritis: Widespread inflammation affecting a large area of the anterior sclera. This type is generally less severe and easier to treat.
- Nodular Anterior Scleritis: Characterized by the presence of distinct, painful nodules on the sclera. These nodules are localized areas of inflammation and can be very tender to touch.
- Necrotizing Anterior Scleritis: The most severe form, leading to tissue damage and potentially causing perforation of the sclera. This type is often associated with severe pain and can be sight-threatening. Necrotizing scleritis can occur with or without inflammation. The non-inflammatory type, known as scleromalacia perforans, is usually painless but can cause significant tissue damage.
- Posterior Scleritis: A less common but serious form affecting the back part of the sclera. It can lead to complications such as retinal detachment, optic neuropathy, and vision loss. Symptoms may include deep eye pain, visual disturbances, and restricted eye movement. Posterior scleritis is more challenging to diagnose due to its location and may require advanced imaging techniques.
Diagnosing Scleritis
Diagnosis involves a comprehensive eye examination by an ophthalmologist. Key diagnostic procedures include:
- Slit-Lamp Examination: Allows detailed examination of the sclera and other eye structures. This tool uses a high-intensity light and a microscope to provide a magnified view of the eye, helping to identify the extent of inflammation and its specific location.
- Ocular Ultrasound: Used particularly for posterior scleritis to visualize the back of the eye. This imaging technique helps in assessing the extent of inflammation and detecting complications like retinal detachment. Ultrasound can provide real-time images and is particularly useful when the sclera is obscured by other structures.
- Blood Tests: To identify underlying systemic conditions or infections. These tests can include complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and specific antibody tests for autoimmune diseases. Blood tests can also help rule out infectious causes of scleritis.
- Imaging Studies: MRI or CT scans may be necessary in complex cases to evaluate the extent of inflammation and involvement of adjacent tissues. These imaging modalities can help in diagnosing orbital inflammation and differentiating scleritis from other conditions like orbital cellulitis. MRI is particularly useful for visualizing soft tissues and detecting subtle changes in the sclera and surrounding structures.
- Fundoscopy: Examination of the interior of the eye, including the retina and optic nerve, to assess for complications like optic neuropathy or retinal detachment.
- Biopsy: In rare cases, a biopsy of the scleral tissue may be required to confirm the diagnosis and rule out other conditions such as malignancies or infections.
Treatment Options
Treatment aims to reduce inflammation, alleviate pain, and address any underlying conditions. Options include:
- Medications:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): For mild cases, NSAIDs such as ibuprofen or naproxen can help reduce pain and inflammation. These drugs are often the first line of treatment for less severe forms of scleritis.
- Corticosteroids: Oral or topical steroids to reduce inflammation. These are typically prescribed for moderate to severe cases and can be administered as eye drops, oral tablets, or injections. Intravenous corticosteroids may be necessary for severe cases.
- Immunosuppressive Drugs: Used in severe cases or when associated with autoimmune diseases. Medications such as methotrexate, azathioprine, or cyclophosphamide can help control the immune response and reduce inflammation. Biologic agents like infliximab or rituximab may be considered for refractory cases.
- Antibiotics/Antifungals/Antivirals: If an infectious cause is identified, appropriate antimicrobial therapy is essential. The choice of medication depends on the specific pathogen involved.
- Treating Underlying Conditions: Managing diseases like rheumatoid arthritis or lupus is crucial in preventing recurrence. This may involve coordinating care with a rheumatologist or other specialists to optimize treatment for the systemic condition. Effective control of the underlying autoimmune disease can significantly reduce the risk of recurrent scleritis.
- Surgery: In rare cases, surgical intervention may be required to repair damaged tissues or address complications. Procedures can include scleral patch grafting to reinforce areas of thinning or perforation and vitrectomy to treat retinal complications. Surgery is typically reserved for cases where medical treatment has failed or when there are significant structural complications.
Preventive Measures and Long-Term Management
Preventing scleritis involves managing underlying risk factors and maintaining overall eye health. Steps include:
- Regular Eye Examinations: Routine check-ups with an ophthalmologist can help detect early signs of inflammation and monitor existing conditions. Early detection and treatment can prevent complications and preserve vision.
- Managing Systemic Diseases: Keeping autoimmune diseases and other underlying conditions well-controlled reduces the risk of scleritis. This may involve regular follow-ups with a rheumatologist and adherence to prescribed medication regimens.
- Protecting the Eyes: Using protective eyewear during activities that pose a risk of eye injury can help prevent trauma-induced scleritis. This includes wearing safety goggles while participating in sports or working with hazardous materials.
- Medication Adherence: Following prescribed treatment plans and medication regimens for both ocular and systemic conditions is crucial for preventing flare-ups and complications. Patients should not discontinue medications without consulting their healthcare provider.
- Lifestyle Modifications: Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, can help support overall health and reduce the risk of autoimmune flare-ups.
Prognosis and Outlook
The prognosis for scleritis varies depending on the underlying cause and the promptness of treatment. With appropriate and timely management, many patients experience significant improvement in symptoms and preservation of vision. However, severe or recurrent cases, particularly those associated with systemic autoimmune diseases, may require long-term treatment and monitoring.
Conclusion
Scleritis is a serious eye condition requiring prompt medical attention. Understanding the symptoms, causes, and treatment options can aid in early diagnosis and effective management. If you experience severe eye pain or persistent redness, seek medical advice immediately. Proper management of underlying conditions and adherence to prescribed treatments can significantly improve outcomes and preserve vision.
By raising awareness and providing detailed information, we hope to empower readers to recognize scleritis early and seek the necessary medical care, ultimately safeguarding their vision and overall ocular health.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Episcleritis is a milder inflammation of the episclera, a thin layer covering the sclera, usually causing less severe pain and redness compared to scleritis. Scleritis involves deeper scleral layers and is often associated with systemic diseases, requiring more intensive treatment.
Yes, adopting a healthy lifestyle, including a balanced diet, regular exercise, stress management, and avoiding smoking, can help support overall health and reduce the risk of autoimmune flare-ups that may trigger scleritis.
While there are no specific dietary recommendations for scleritis, maintaining a balanced diet rich in anti-inflammatory foods like fruits, vegetables, omega-3 fatty acids, and whole grains can support overall health and potentially reduce inflammation.
Scleritis can significantly impact daily life, causing severe pain, light sensitivity, and visual disturbances. These symptoms can interfere with routine activities, work, and quality of life, making prompt and effective treatment essential.
There may be a genetic predisposition, especially if there is a family history of autoimmune diseases. However, scleritis itself is not directly inherited, and environmental and immune factors also play significant roles.
While stress is not a direct cause of scleritis, it can exacerbate autoimmune conditions and potentially trigger flare-ups in individuals with underlying autoimmune diseases, thereby increasing the risk of scleritis.
Untreated scleritis can lead to severe complications, including scleral thinning and perforation, corneal involvement, uveitis, glaucoma, cataracts, and permanent vision loss due to damage to ocular structures.
Yes, scleritis can recur, especially if the underlying systemic condition is not well-managed. Ongoing monitoring and treatment of autoimmune diseases are crucial to reducing the risk of recurrence.
An ophthalmologist is essential in diagnosing and managing scleritis, providing comprehensive eye examinations, prescribing appropriate treatments, and coordinating care with other specialists for systemic conditions.
Research is ongoing to find new treatments for scleritis, including biologic therapies targeting specific immune pathways. Clinical trials and advancements in immunosuppressive drugs offer hope for more effective and targeted treatments in the future.
news via inbox
Subscribe here to get latest updates !