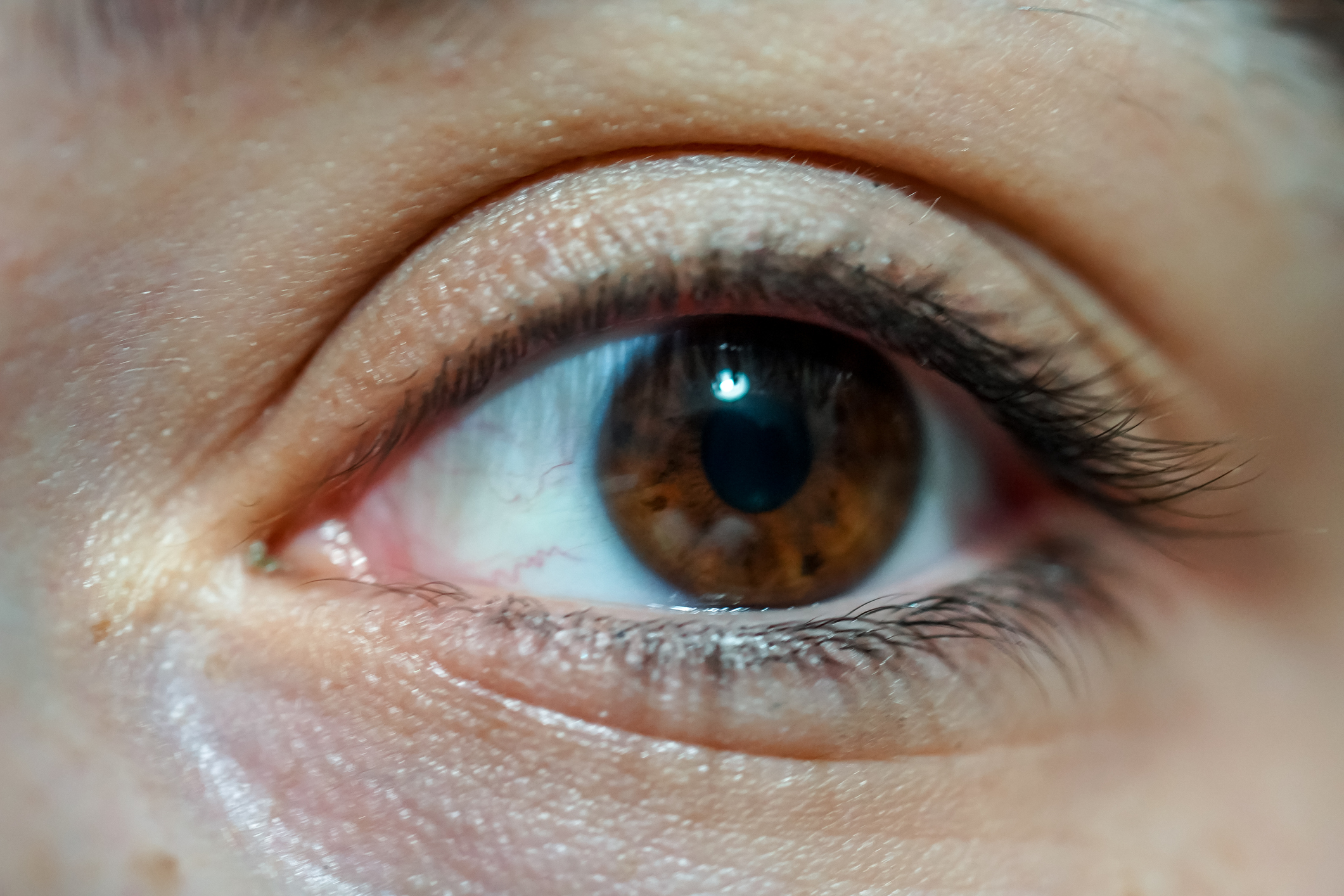
A Closer Look at Corneal Edema
Corneal edema is a condition characterized by swelling of the cornea, the clear front part of the eye. This article aims to provide a comprehensive and empathetic guide to corneal edema, covering its causes, symptoms, when to seek medical attention, diagnosis, and management strategies.
Overview of Corneal Edema
Corneal edema refers to the swelling of the cornea, the clear front surface of the eye. The cornea plays a crucial role in focusing light onto the retina, and any disruption in its clarity can lead to visual disturbances. Corneal edema results from an accumulation of fluid within the corneal tissues, impacting its transparency and causing a range of symptoms.
Causes
- Endothelial Dysfunction: The corneal endothelium is responsible for maintaining the balance of fluid in the cornea. Dysfunction of the endothelial cells, often due to aging, trauma, or certain eye surgeries, can lead to corneal edema.
- Fuchs’ Endothelial Dystrophy: A genetic condition where the corneal endothelial cells progressively deteriorate, leading to corneal edema.
- Corneal Infections: Bacterial, viral, or fungal infections can cause inflammation and fluid accumulation in the cornea, leading to edema.
- Corneal Trauma: Injuries, scratches, or trauma to the cornea can disrupt its normal structure and result in swelling.
- Iatrogenic Causes: Complications from eye surgeries, such as cataract surgery or refractive surgery, can sometimes lead to corneal edema.
- Glaucoma Medications: Long-term use of certain eye medications, especially those containing preservatives, can contribute to corneal edema.
- Inflammatory Eye Conditions: Diseases like uveitis or iritis can cause inflammation in the eye, leading to corneal edema.
Symptoms
- Blurred Vision: Corneal edema can cause significant visual disturbances, including blurred or hazy vision.
- Increased Sensitivity to Light (Photophobia): Irritation from corneal edema can make the eyes more sensitive to light.
- Halos Around Lights: Individuals with corneal edema may see halos or glares around lights, especially at night.
- Eye Discomfort or Pain: Mild to moderate discomfort, a feeling of pressure, or occasional pain can be associated with corneal edema.
- Watery Eyes: Excessive tearing or watering of the eyes may occur as a response to corneal irritation.
- Reduced Visual Clarity: The ability to see fine details may be compromised due to the cloudy appearance of the cornea.
When to Seek Medical Attention
- Sudden Changes in Vision: Any sudden and significant changes in vision, especially if accompanied by pain or discomfort, require immediate medical attention.
- Eye Trauma: Seek prompt medical help if the cornea is injured, scratched, or if a foreign body is embedded in the eye.
- Persistent Eye Discomfort: If symptoms like pain, redness, or irritation persist, it is crucial to consult with an eye care professional.
- Light Sensitivity: Increased sensitivity to light, particularly if it is sudden or severe, should be evaluated promptly.
- Corneal Infections: Suspected or confirmed corneal infections, often characterized by redness, discharge, and vision changes, require urgent medical attention.
- Postoperative Complications: If corneal edema develops after eye surgery, such as cataract surgery, it is essential to contact the surgeon for evaluation and management.
- Known Corneal Conditions: Individuals with pre-existing corneal conditions or a history of eye surgery should be vigilant about changes in vision and promptly seek medical attention if concerns arise.
Early diagnosis and appropriate management of the underlying cause of corneal edema are crucial for preventing complications and preserving vision. If you experience any concerning symptoms related to your eyes, consulting with an eye care professional is recommended.
Diagnosis
- Comprehensive Eye Examination: A thorough eye examination, including visual acuity testing, slit-lamp biomicroscopy, and evaluation of the corneal thickness, is essential for diagnosing corneal edema.
- Corneal Topography: This imaging technique maps the surface curvature of the cornea, providing detailed information about its shape and identifying areas of swelling.
- Pachymetry: Measurement of corneal thickness using ultrasound or optical methods helps assess the extent of swelling and may contribute to the diagnosis.
- Endothelial Cell Count: Evaluating the density of corneal endothelial cells can provide insights into the health of the corneal endothelium, which is crucial for maintaining corneal transparency.
- Gonioscopy: This test assesses the drainage angle of the eye and helps rule out conditions like glaucoma, which can contribute to corneal edema.
- Corneal Dye Staining: Using dyes like fluorescein can help visualize corneal abrasions or defects contributing to edema.
- Intraocular Pressure Measurement: Checking intraocular pressure is important, especially if glaucoma is suspected as a cause of corneal edema.
Management Strategies
- Topical Medications: Depending on the underlying cause, eye drops may be prescribed to address inflammation, control infection, or manage intraocular pressure.
- Hyperosmotic Agents: These medications help draw excess fluid out of the cornea, reducing swelling. Examples include hypertonic saline or oral glycerin.
- Steroid Eye Drops: In cases of inflammation, steroid eye drops may be prescribed to reduce swelling and inflammation in the cornea.
- Bandage Contact Lenses: Soft or therapeutic contact lenses can be used to protect the cornea and promote healing, especially in cases of corneal abrasions.
- Surgical Procedures: In some cases, surgical interventions may be necessary. This can include corneal transplantation (keratoplasty) or procedures to address underlying conditions contributing to edema.
- Management of Underlying Conditions: Identifying and treating the underlying cause of corneal edema is crucial. For example, managing glaucoma or addressing endothelial dysfunction may be part of the overall treatment plan.
- Moisture Chamber Goggles: These specialized goggles create a humid environment around the eye, which can be beneficial in cases of corneal exposure or persistent dryness.
- Artificial Tears: Lubricating eye drops can help alleviate symptoms associated with dryness and improve comfort.
Demographics More Affected
- Age: Corneal edema can affect individuals of all ages, but certain causes, such as Fuchs’ endothelial dystrophy, may be more prevalent in older adults.
- Postoperative Patients: Individuals who have undergone eye surgery, particularly procedures like cataract surgery, may be more prone to postoperative corneal edema.
- Contact Lens Wearers: Improper use or extended wear of contact lenses can contribute to corneal edema, especially if hygiene practices are not followed.
- Patients with Pre-existing Eye Conditions: Individuals with conditions such as Fuchs’ endothelial dystrophy, corneal infections, or inflammatory eye diseases may be more susceptible to corneal edema.
- Those with Glaucoma: Elevated intraocular pressure in glaucoma can contribute to corneal edema, especially if the condition is not well-managed.
- Genetic Factors: Conditions with a genetic component, such as Fuchs’ endothelial dystrophy, may affect certain populations more than others.
Understanding the demographics more affected by corneal edema helps guide preventive measures, early detection, and appropriate management strategies. Regular eye examinations and prompt medical attention for symptoms are crucial in maintaining corneal health and preserving vision.
Conclusion
Understanding the causes, recognizing common symptoms, and exploring treatment options are essential components of addressing corneal edema. By prioritizing eye health and seeking timely medical attention, individuals can take proactive steps to preserve their vision and maintain overall well-being.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
The impact on vision varies depending on the severity of corneal edema and the underlying cause. Timely intervention and appropriate management can prevent permanent vision loss.
While corneal edema can occur at any age, certain conditions leading to edema, like Fuchs’ dystrophy, may be more common in older adults.
Improper use, hygiene, or extended wear of contact lenses may contribute to corneal edema. Following recommended practices is essential to prevent complications.
The approach to managing corneal edema depends on the underlying cause. In some cases, medical treatments may help improve or stabilize the condition without surgery.
Yes, corneal edema can affect one or both eyes, depending on the underlying cause and contributing factors.
Corneal edema itself may not cause pain, but underlying conditions contributing to edema, such as eye injuries or inflammatory conditions, can be associated with pain or discomfort.
Over-the-counter eye drops may provide temporary relief for some symptoms but are not a specific treatment for corneal edema. Prescription medications and professional guidance are often necessary.
Lifestyle changes may include protecting the eyes from injury, following proper contact lens hygiene, and managing underlying health conditions that contribute to corneal edema.
Corneal edema can be temporary, especially if it is a result of a reversible cause like eye surgery or trauma. However, chronic conditions may lead to persistent edema.
Yes, corneal edema can be a symptom of underlying eye conditions such as Fuchs’ dystrophy, uveitis, or complications from eye surgery.
news via inbox
Subscribe here to get latest updates !