A Comprehensive Guide to Corneal Transplant Surgery
Introduction
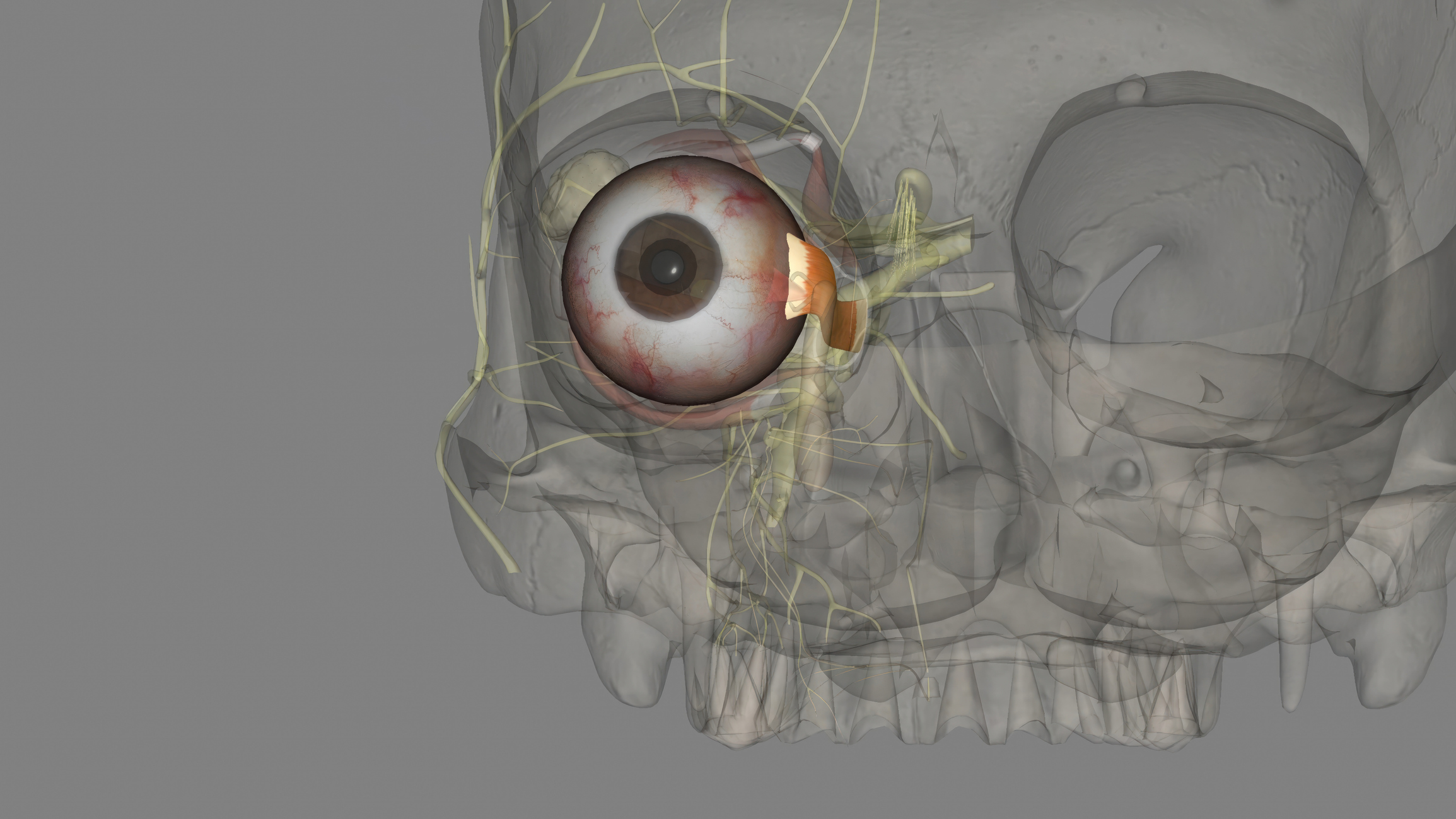
Corneal transplant surgery, also known as keratoplasty, is a transformative procedure designed to restore vision by replacing a damaged or diseased cornea with a healthy donor cornea. As the clear, outermost layer of the eye, the cornea plays a critical role in refracting light and focusing images onto the retina, facilitating clear vision. When the cornea becomes compromised due to injury, infection, or disease, it can lead to visual impairment, discomfort, and diminished quality of life. Corneal transplant surgery offers hope and a path to improved vision for individuals facing such challenges. This comprehensive guide aims to provide a thorough understanding of corneal transplant surgery, from the intricacies of the procedure itself to the recovery process and long-term outcomes.
Exploring the Different Types of Corneal Transplant Surgery
Penetrating Keratoplasty (PKP)
PKP involves replacing the entire thickness of the cornea with a donor cornea. This procedure is suitable for individuals with significant corneal damage, such as advanced scarring, severe keratoconus, or certain inherited corneal disorders. PKP is typically recommended when the majority of the cornea is affected, requiring complete replacement to restore vision.
Partial Thickness Transplants (DSAEK and DMEK)
Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) and Descemet’s Membrane Endothelial Keratoplasty (DMEK) are innovative procedures that target specific layers of the cornea, primarily the endothelium and Descemet’s membrane. These surgeries are often preferred for conditions affecting the corneal endothelium, such as Fuchs’ endothelial dystrophy, where only the innermost layers of the cornea are damaged. DSAEK and DMEK offer the advantage of faster recovery times and potentially better visual outcomes compared to PKP, as they preserve more of the patient’s corneal tissue.
Preparation for Surgery and What to Expect
Who Needs Corneal Transplant Surgery:
Corneal transplant surgery may be recommended for individuals experiencing vision impairment or discomfort due to various corneal conditions, including but not limited to:
- Corneal scarring from injury or infection
- Keratoconus (a progressive thinning and bulging of the cornea)
- Corneal dystrophies (inherited disorders affecting the cornea)
- Corneal edema or swelling, often due to endothelial dysfunction
- Corneal degeneration or thinning disorders
Preoperative Evaluation:
Before undergoing corneal transplant surgery, patients undergo a comprehensive evaluation by an ophthalmologist to assess the extent of corneal damage and determine their candidacy for the procedure. This evaluation typically includes:
- A thorough medical history to identify any underlying conditions that may affect surgical outcomes.
- Visual acuity testing to evaluate the severity of vision loss.
- Corneal imaging techniques such as corneal topography or optical coherence tomography (OCT) to assess corneal shape, thickness, and integrity.
- Evaluation of ocular health to ensure there are no contraindications to surgery, such as active eye infections or uncontrolled eye inflammation.
Donor Cornea Selection:
Once a patient is deemed a suitable candidate for corneal transplant surgery, the surgeon coordinates with eye banks to select a donor cornea that matches the patient’s corneal size and shape as closely as possible. Donor corneas undergo rigorous screening and testing to ensure they are free from infectious diseases and suitable for transplantation.
Surgery Day:
On the day of surgery, patients receive anesthesia to ensure comfort during the procedure. The surgeon performs the chosen type of corneal transplant, meticulously removing the damaged corneal tissue and replacing it with the donor cornea. The surgery typically takes one to two hours, depending on the complexity of the procedure.
Navigating the Recovery Process and Postoperative Care
- Immediate Post-op Care: After surgery, you’ll spend time in a recovery area where your vital signs and eye condition will be closely monitored. It’s normal to experience some discomfort, blurred vision, and light sensitivity immediately following surgery.
- Medication Regimen: Your surgeon will prescribe a regimen of eye drops to prevent infection, reduce inflammation, and promote healing. It’s essential to adhere to this medication regimen diligently and follow your doctor’s instructions regarding frequency and duration.
- Follow-up Visits: Regular follow-up appointments with your ophthalmologist are crucial for monitoring your progress, evaluating the healing process, and assessing your visual acuity. During these visits, your doctor may adjust your medication regimen and provide guidance on activities and precautions.
Long-Term Outlook and Expectations
- Visual Rehabilitation: While individual experiences vary, many patients experience significant improvement in their vision following corneal transplant surgery. It’s important to have realistic expectations, as visual recovery may take several months, and optimal outcomes may continue to improve over time.
- Potential Complications and Management: Although corneal transplant surgery is generally safe, there are risks of complications such as graft rejection, infection, or glaucoma. Prompt recognition and treatment of these complications are essential for maximizing the success of the transplant and preserving vision.
Conclusion
Corneal transplant surgery represents a beacon of hope for individuals facing vision impairment due to corneal damage or disease. By understanding the intricacies of the procedure, preparing adequately, and diligently adhering to postoperative care instructions, patients can embark on a journey toward improved vision and enhanced quality of life. If you’re considering corneal transplant surgery, consult with your eye care provider to discuss your options, address any concerns, and embark on a personalized treatment plan tailored to your unique needs and circumstances.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Recovery time varies depending on the type of surgery and individual healing factors. Typically, patients experience improvement in vision over several weeks to months post-surgery.
It’s essential to refrain from driving until your surgeon confirms that your vision meets the legal requirements for driving. This typically occurs after your vision stabilizes, and any restrictions on activities are lifted.
Your surgeon will provide specific guidelines regarding physical activities post-surgery. Initially, you may need to avoid strenuous activities, heavy lifting, and contact sports to prevent injury to the eye during the healing process.
Symptoms of corneal transplant rejection may include increased eye redness, pain, sensitivity to light, decreased vision, or a sudden onset of vision changes. If you experience any of these symptoms, contact your surgeon immediately for evaluation.
The longevity of a corneal transplant varies among individuals and depends on various factors, including the underlying condition, surgical technique, and postoperative care. With proper care and monitoring, corneal transplants can last many years or even a lifetime.
In some cases, individuals may be able to wear contact lenses after corneal transplant surgery to further improve vision. However, this decision depends on factors such as corneal shape, stability of the transplant, and your surgeon’s recommendations.
Although corneal transplant surgery is generally safe, potential risks include infection, graft rejection, elevated intraocular pressure (glaucoma), and astigmatism. Your surgeon will discuss these risks with you and take steps to minimize them.
Performing corneal transplant surgery on both eyes simultaneously is uncommon due to the increased risk and potential challenges associated with postoperative care. Your surgeon will determine the most appropriate approach based on your individual circumstances.
While some patients experience improved vision after corneal transplant surgery, many still require glasses or contact lenses to achieve optimal visual acuity, especially for activities such as reading or driving.
Following corneal transplant surgery, it’s essential to prioritize eye health by avoiding activities that may increase the risk of injury or infection, maintaining a healthy lifestyle, and attending regular follow-up appointments with your eye care provider.
news via inbox
Subscribe here to get latest updates !