A Journey with Retinal Vein Occlusion
Retinal Vein Occlusion, a condition affecting the blood vessels in the eye, can lead to vision disturbances. This article aims to provide a comprehensive understanding of Retinal Vein Occlusion, covering symptoms, causes, when to seek medical attention, risk factors, prevention strategies, available treatments, and follow-up care for both adults and children.
Overview of Retinal Vein Occlusion
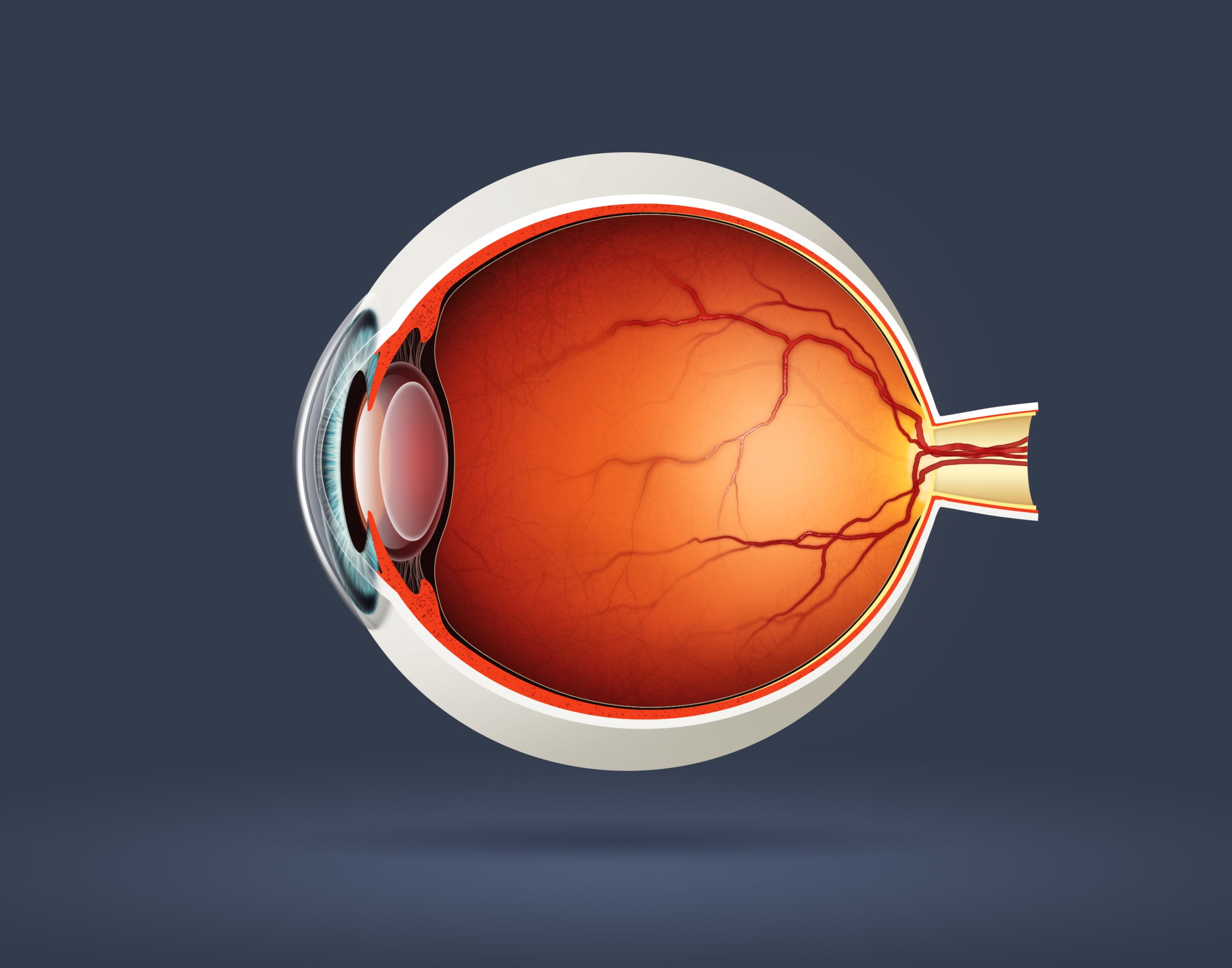
Retinal vein occlusion (RVO) is a vascular disorder that occurs when there is a blockage or obstruction in the veins that carry blood away from the retina. The retina is a crucial part of the eye responsible for converting light into neural signals. When a vein in the retina becomes blocked, it can lead to a range of symptoms and potentially cause vision impairment.
Symptoms
- Sudden Vision Loss: One of the hallmark symptoms is a sudden onset of blurred or distorted vision in one eye.
- Floaters: Dark spots or floaters may appear in the visual field.
- Visual Field Defects: Peripheral vision may be affected, leading to the perception of missing areas in the visual field.
- Pain or Discomfort: Some individuals may experience pain or discomfort in the eye.
- Changes in Color Vision: Perception of colors may be altered.
It’s important to note that the severity of symptoms can vary, and some individuals with RVO may not experience noticeable symptoms until complications arise.
Causes
Retinal vein occlusion can be classified into two main types:
- Central Retinal Vein Occlusion (CRVO): This occurs when the main vein of the retina is blocked. The exact cause is often multifactorial and may involve factors such as hypertension, diabetes, and blood clotting disorders.
- Branch Retinal Vein Occlusion (BRVO): This type involves the blockage of one of the smaller branch veins of the retina. Common causes include atherosclerosis, where cholesterol deposits narrow the blood vessels, and other vascular diseases.
Additional risk factors for retinal vein occlusion include:
- Age: The risk increases with age.
- Hypertension: High blood pressure is a significant risk factor.
- Diabetes: Individuals with diabetes are more prone to vascular complications.
- Glaucoma: Increased intraocular pressure may contribute to vein compression.
- Smoking: Tobacco use is associated with an increased risk.
When to See a Doctor
Prompt medical attention is crucial if any symptoms suggestive of retinal vein occlusion are experienced. It is recommended to see a doctor:
- Sudden Vision Changes: If there is a sudden onset of vision changes, especially if it involves partial or complete loss of vision in one eye.
- Persistent Floaters or Flashing Lights: The presence of persistent floaters or flashing lights in the vision should be evaluated.
- Eye Pain or Discomfort: Any unexplained pain or discomfort in the eye should prompt a visit to an eye care professional.
- Risk Factors Present: Individuals with risk factors such as hypertension, diabetes, or a history of vascular diseases should be vigilant and seek medical attention if they experience visual disturbances.
What Happens Because of Retinal Vein Occlusion
Retinal vein occlusion (RVO) disrupts the normal blood flow in the retina, leading to a range of consequences:
- Vision Impairment: The primary outcome is a varying degree of vision impairment, ranging from mild blurriness to severe visual loss, depending on the location and extent of the vein occlusion.
- Macular Edema: Swelling of the macula, the central part of the retina responsible for detailed vision, can occur, leading to further visual distortion.
- Ischemia: Reduced blood flow to parts of the retina can result in ischemia, potentially causing the formation of new, abnormal blood vessels or other complications.
- Retinal Hemorrhage: The blocked blood vessels may leak, leading to retinal hemorrhage and further compromising vision.
- Glaucoma: RVO can be associated with an increased risk of developing glaucoma, a condition characterized by elevated intraocular pressure that can damage the optic nerve.
Risk Factors
Several factors increase the risk of developing retinal vein occlusion:
- Age: The risk increases with age, with RVO being more common in individuals over 50.
- Hypertension: High blood pressure is a significant risk factor for RVO.
- Diabetes: Individuals with diabetes are more prone to vascular complications, including RVO.
- Hyperlipidemia: Elevated levels of cholesterol and triglycerides are associated with an increased risk.
- Smoking: Tobacco use is a modifiable risk factor that contributes to vascular diseases, including RVO.
- Glaucoma: Individuals with glaucoma may be at a higher risk of RVO.
Complications
Complications of retinal vein occlusion include:
- Macular Edema: Swelling in the macula can lead to persistent visual impairment.
- Neovascularization: Abnormal blood vessel growth can occur, increasing the risk of bleeding and scarring.
- Vision Loss: In severe cases, prolonged or untreated RVO can lead to permanent vision loss.
- Glaucoma: Increased intraocular pressure associated with RVO can contribute to the development or progression of glaucoma.
Prevention
While some risk factors are not modifiable, certain measures can help reduce the risk of retinal vein occlusion:
- Blood Pressure Control: Maintaining healthy blood pressure levels through lifestyle modifications or medication.
- Blood Sugar Management: For individuals with diabetes, effective management of blood sugar levels is essential.
- Cholesterol Management: Controlling cholesterol levels through a healthy diet, exercise, and medication when necessary.
- Smoking Cessation: Quitting smoking can significantly reduce the risk of vascular diseases.
- Regular Eye Exams: Routine eye examinations can help detect and manage conditions like hypertension, diabetes, and glaucoma, contributing to the prevention of RVO.
Diagnosis
Diagnosing retinal vein occlusion involves a thorough eye examination, which may include:
- Dilated Eye Exam: Examining the retina and optic nerve for signs of vein occlusion.
- Fluorescein Angiography: Injecting a dye into the bloodstream to highlight blood vessels and identify areas of blockage.
- Optical Coherence Tomography (OCT): Producing detailed cross-sectional images of the retina to assess macular edema and other structural changes.
- Blood Tests: Checking for underlying conditions such as diabetes or hyperlipidemia.
Early diagnosis is crucial for the timely management of RVO and the prevention of complications that could lead to permanent vision loss.
Treatment Options
The management of retinal vein occlusion (RVO) aims to address the underlying causes, manage complications, and preserve or improve vision. Treatment options may include:
- Anti-VEGF Injections: Intravitreal injections of anti-vascular endothelial growth factor (VEGF) medications, such as ranibizumab or aflibercept, are often used to reduce macular edema and inhibit abnormal blood vessel growth.
- Corticosteroids: Intravitreal injections or sustained-release implants of corticosteroids may be employed to decrease inflammation and reduce macular edema.
- Laser Therapy: Laser photocoagulation may be used to treat areas of ischemia and prevent the growth of abnormal blood vessels. This approach is particularly applicable in cases of retinal vein occlusion associated with neovascularization.
- Retinal Surgery: In advanced cases, vitrectomy surgery may be considered to address complications such as vitreous hemorrhage or to remove scar tissue affecting the retina.
Medications
Several medications may be prescribed to manage retinal vein occlusion and associated complications:
- Antiplatelet Agents: Medications like aspirin may be recommended to reduce the risk of blood clots and improve blood flow.
- Anticoagulants: In some cases, anticoagulant medications may be prescribed to prevent further clot formation.
- Intraocular Steroids: Steroids may be administered either through injections or sustained-release implants to reduce inflammation and macular edema.
- Pain Management: Analgesics or pain-relief medications may be recommended if individuals experience eye pain or discomfort.
Follow-Up Care
Regular follow-up care is essential to monitor the progression of retinal vein occlusion, assess the effectiveness of treatment, and address any emerging complications. Follow-up care may include:
- Ongoing Monitoring: Regular eye examinations, visual acuity assessments, and imaging studies to monitor changes in the retina and assess treatment efficacy.
- Adjustment of Treatment: Depending on the response to initial interventions, the treatment plan may be modified to optimize outcomes.
- Blood Pressure Management: Controlling blood pressure and other systemic conditions through medication and lifestyle modifications.
- Lifestyle Counseling: Providing guidance on lifestyle changes, including smoking cessation, a healthy diet, and regular exercise to mitigate risk factors.
Demographics More Susceptible
Conclusion
Understanding the causes, recognizing symptoms, and exploring management options are key aspects of navigating Retinal Vein Occlusion. By being aware of potential risk factors and taking proactive steps, individuals can contribute to maintaining their eye health and seeking timely intervention if needed.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
While there may be a genetic predisposition, Retinal Vein Occlusion is not typically considered a hereditary condition. Lifestyle factors and other health conditions play significant roles.
RVO can be associated with systemic conditions like hypertension and diabetes. Comprehensive medical evaluations may be conducted to assess overall health.
Medications to dissolve blood clots may not be routinely used for Retinal Vein Occlusion. Treatment often focuses on addressing swelling and inflammation.
Individuals with Retinal Vein Occlusion should have regular follow-up appointments with their eye care professional to monitor the condition and address any changes in vision.
While Retinal Vein Occlusion can result in vision changes, including severe vision loss, complete blindness is rare. Timely and appropriate management can help preserve vision.
Yes, Retinal Vein Occlusion can occur in one or both eyes. The risk of it occurring in the other eye is increased if already diagnosed in one eye.
Long-term complications may include vision changes, particularly if macular edema is present. Regular follow-ups with an eye care professional help monitor and manage any complications.
Adopting a healthy lifestyle, including regular exercise, a balanced diet, and managing systemic conditions, can contribute to reducing the risk of RVO.
Surgery is not typically the first-line treatment for RVO. Non-surgical interventions such as injections and laser therapy are often considered first.
While the effects of Retinal Vein Occlusion may be managed, complete reversal of the condition may not be possible. Timely intervention can help preserve remaining vision.
news via inbox
Subscribe here to get latest updates !