Acute Retinal Necrosis Syndrome: Symptoms and Treatment
Introduction
Acute Retinal Necrosis Syndrome (ARN) is a rare but serious ocular condition characterized by inflammation and necrosis (tissue death) of the retina, the light-sensitive layer at the back of the eye responsible for transmitting visual information to the brain. ARN typically manifests as a rapidly progressing and potentially blinding disease if not promptly diagnosed and treated. It primarily affects the outer layers of the retina, leading to severe vision impairment or even permanent vision loss.
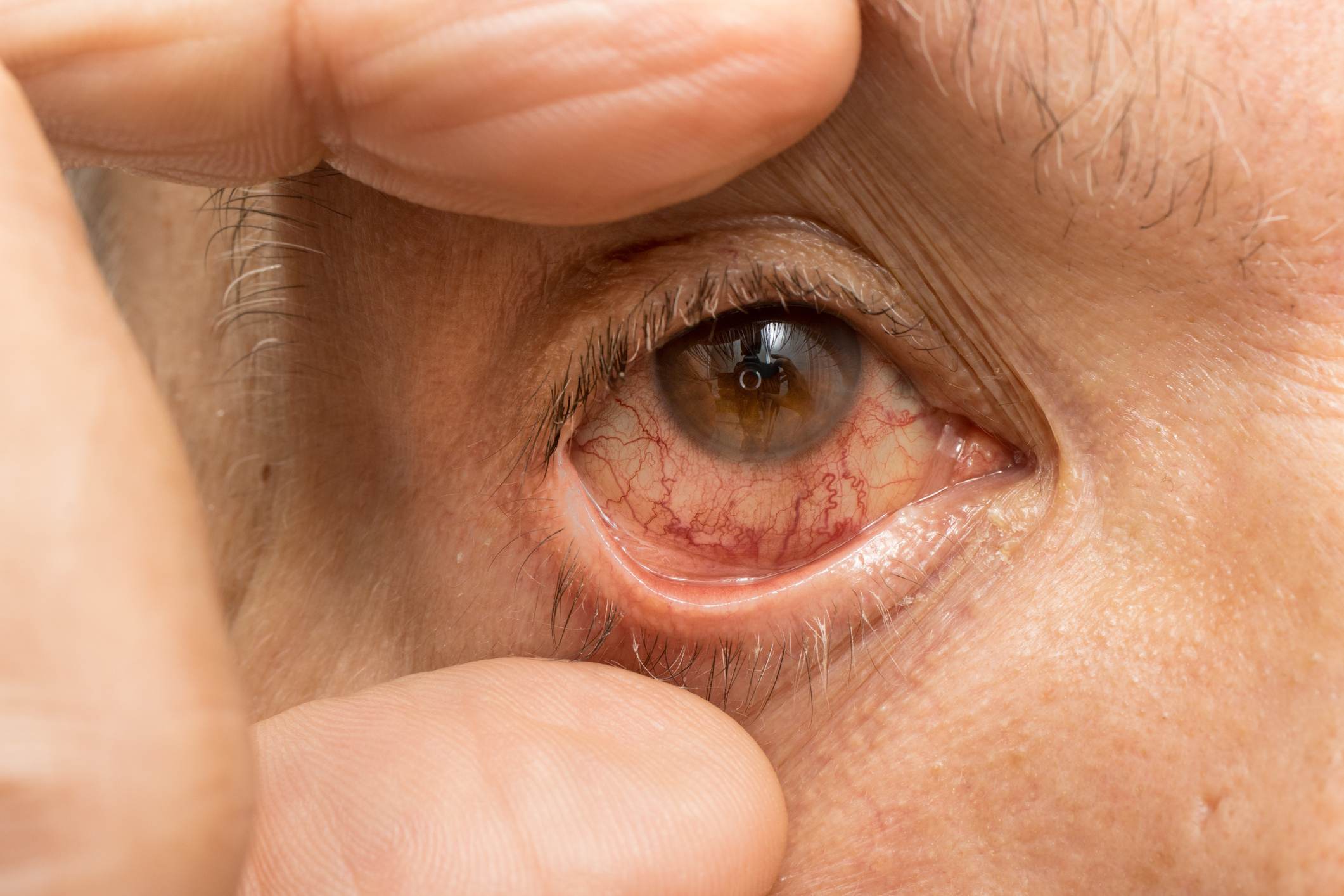
The onset of ARN is often sudden and may be accompanied by symptoms such as floaters (dark spots or specks drifting in the vision), flashes of light (photopsia), eye pain, redness, and blurred or decreased vision. The condition can affect one or both eyes and is frequently associated with viral infections, particularly those caused by herpesviruses such as herpes simplex virus (HSV) and varicella-zoster virus (VZV).
While ARN is relatively rare, it tends to occur more frequently in individuals with compromised immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapy. Early recognition and intervention are crucial to prevent irreversible damage to the retina and preserve visual function.
Causes of Acute Retinal Necrosis Syndrome
The primary cause of Acute Retinal Necrosis Syndrome is viral infection, most commonly associated with herpesviruses, including:
- Herpes Simplex Virus (HSV): Both HSV type 1 (HSV-1) and HSV type 2 (HSV-2) have been implicated in the development of ARN. HSV-1 is typically associated with oral lesions (cold sores), while HSV-2 is often associated with genital lesions. However, either virus can affect the eyes, leading to severe ocular complications.
- Varicella-Zoster Virus (VZV): VZV is responsible for causing chickenpox (varicella) and shingles (herpes zoster). Reactivation of the virus can result in ocular inflammation and necrosis, leading to ARN.
These viruses can enter the eye through various routes, such as direct inoculation, reactivation from latent infection, or hematogenous spread. Once inside the eye, the viruses trigger a robust inflammatory response, leading to tissue damage and necrosis of the retina.
Other risk factors for developing ARN include immunosuppression (e.g., HIV/AIDS, organ transplantation), previous ocular surgery or trauma, and a history of herpetic infections.
Diagnosis of Acute Retinal Necrosis Syndrome
Diagnosing Acute Retinal Necrosis Syndrome involves a thorough evaluation by an ophthalmologist, typically including the following steps:
- Visual Acuity Testing: Assessing the clarity and sharpness of vision using eye charts to detect any visual impairment.
- Slit-Lamp Examination: A specialized microscope equipped with a bright light source is used to examine the external and internal structures of the eye, including the retina, optic nerve, and anterior chamber.
- Dilated Fundus Examination: Dilating the pupil allows for a detailed examination of the retina and optic nerve using a direct or indirect ophthalmoscope. This helps identify characteristic signs of ARN, such as retinal inflammation, necrosis, hemorrhage, or detachment.
- Fluorescein Angiography: Injecting a fluorescent dye into a vein in the arm allows for visualization of blood flow within the retina. This test helps identify areas of retinal ischemia (lack of blood flow) or leakage, which are common findings in ARN.
- Polymerase Chain Reaction (PCR) Testing: Extracting ocular fluid samples, such as aqueous or vitreous humor, for laboratory analysis can help detect viral DNA and confirm the presence of herpesvirus infection. PCR testing is highly sensitive and specific for diagnosing ARN.
These diagnostic tests aid in confirming the diagnosis of ARN and differentiating it from other ocular conditions with similar symptoms.
Treatment of Acute Retinal Necrosis Syndrome
The treatment approach for Acute Retinal Necrosis Syndrome aims to suppress viral replication, reduce inflammation, and prevent further damage to the retina. Commonly used treatment modalities include:
- Antiviral Medications: Oral or intravenous administration of antiviral drugs such as acyclovir, valacyclovir, or foscarnet is the cornerstone of ARN treatment. These medications inhibit viral replication and help control the spread of infection within the eye.
- Corticosteroids: Topical or systemic administration of corticosteroids may be used to reduce inflammation and alleviate symptoms associated with ARN. However, the use of corticosteroids should be carefully monitored due to the risk of exacerbating viral replication or inducing complications such as intraocular pressure elevation.
- Intravitreal Injections: Direct injection of antiviral medications (e.g., ganciclovir) or corticosteroids into the vitreous cavity allows for targeted delivery of high concentrations of medication to the affected area. Intravitreal injections are often reserved for severe or refractory cases of ARN.
- Retinal Detachment Surgery: In cases where ARN leads to complications such as retinal detachment, surgical intervention may be necessary to reattach the retina and restore visual function. Surgical techniques may include vitrectomy, scleral buckling, or pneumatic retinopexy, depending on the extent and severity of retinal detachment.
The choice of treatment modality depends on factors such as the severity of the condition, the extent of retinal involvement, and the patient’s overall health status. Close collaboration between the ophthalmologist and infectious disease specialist is essential to optimize treatment outcomes and minimize the risk of complications.
Prognosis
The prognosis for ARN varies depending on factors such as the severity of the condition, the promptness of diagnosis, and the effectiveness of treatment. While some individuals may experience significant visual recovery with early intervention, others may suffer permanent vision loss despite aggressive therapy. Regular follow-up appointments with an ophthalmologist are essential to monitor the progression of the disease and adjust treatment as needed.
Conclusion
Acute Retinal Necrosis Syndrome is a serious ocular condition characterized by viral-induced inflammation and necrosis of the retina. Recognizing the symptoms, seeking prompt medical attention, and initiating appropriate treatment are crucial steps in preserving vision and minimizing the impact of this sight-threatening condition. By understanding the symptoms, causes, diagnosis, and treatment options for ARN, individuals can empower themselves to take proactive measures in managing their ocular health and optimizing visual outcomes.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
If you experience symptoms such as sudden vision changes, floaters, or eye pain, it’s crucial to seek immediate medical attention from an ophthalmologist. Early diagnosis and treatment can help preserve vision and prevent complications.
While antiviral medications and corticosteroids are the primary treatments for ARN, some individuals may benefit from adjunctive therapies such as immunomodulatory agents or intravenous immunoglobulin (IVIG).
Recurrence of ARN is possible, particularly in individuals with a compromised immune system. Close monitoring and early intervention are essential for managing recurrent episodes.
Maintaining a healthy lifestyle, including proper nutrition and regular exercise, may support overall eye health. Additionally, avoiding triggers that can exacerbate viral infections, such as stress or UV exposure, may be beneficial.
The long-term effects of ARN can vary, with some individuals experiencing partial or complete vision loss despite treatment. Regular follow-up with an ophthalmologist is essential for monitoring any complications and adjusting treatment as needed.
Yes, ARN can affect one or both eyes simultaneously or sequentially. Bilateral involvement may occur in up to one-third of cases.
While ARN can affect individuals of any age, it is more commonly observed in adults, particularly those with compromised immune systems.
Symptoms of ARN can develop rapidly within days to weeks after viral exposure, but the timeline may vary depending on individual factors and the specific virus involved.
ARN itself is not contagious, but the viruses that cause it (such as HSV or VZV) can be transmitted through close contact with an infected individual during active viral shedding.
Currently, there are no specific preventive measures for ARN. However, maintaining overall eye health and promptly treating any ocular infections may reduce the risk of complications.
news via inbox
Subscribe here to get latest updates !