Biomechanics Research for Understanding Eye Movement Disorders
Introduction
Biomechanics, the study of the mechanical aspects of living organisms, plays a crucial role in understanding various physiological processes, including eye movements. Eye movement disorders encompass a wide range of conditions that affect the normal function of the ocular muscles, nerves, or brain regions responsible for controlling eye movements. Biomechanics research offers valuable insights into the underlying mechanisms of these disorders, paving the way for more effective diagnosis, treatment, and rehabilitation strategies. In this article, we delve into the significance of biomechanics research in unraveling the complexities of eye movement disorders.
Understanding Normal Eye Movements
Biomechanics research helps elucidate the intricate interplay between muscles, nerves, and brain regions involved in orchestrating precise eye movements. By studying the biomechanical properties of ocular structures and their coordination, researchers gain insights into how healthy eyes move and function.
Techniques such as motion capture systems, electromyography (EMG), and computational modeling allow researchers to analyze the dynamics of eye movements in both static and dynamic conditions. These tools provide quantitative data on factors such as muscle activation patterns, force generation, and coordination between different eye muscles.
Characterizing Eye Movement Disorders
Biomechanics research plays a pivotal role in characterizing the biomechanical abnormalities associated with various eye movement disorders. Conditions such as strabismus (ocular misalignment), nystagmus (involuntary eye movements), and oculomotor apraxia (impaired voluntary eye movements) present unique biomechanical challenges that can be investigated using advanced biomechanical techniques.
By analyzing deviations from normal eye movement patterns, researchers can identify specific biomechanical deficits underlying different disorders. This knowledge is instrumental in refining diagnostic criteria, predicting disease progression, and developing targeted interventions for affected individuals.
Advancing Diagnostic and Therapeutic Strategies
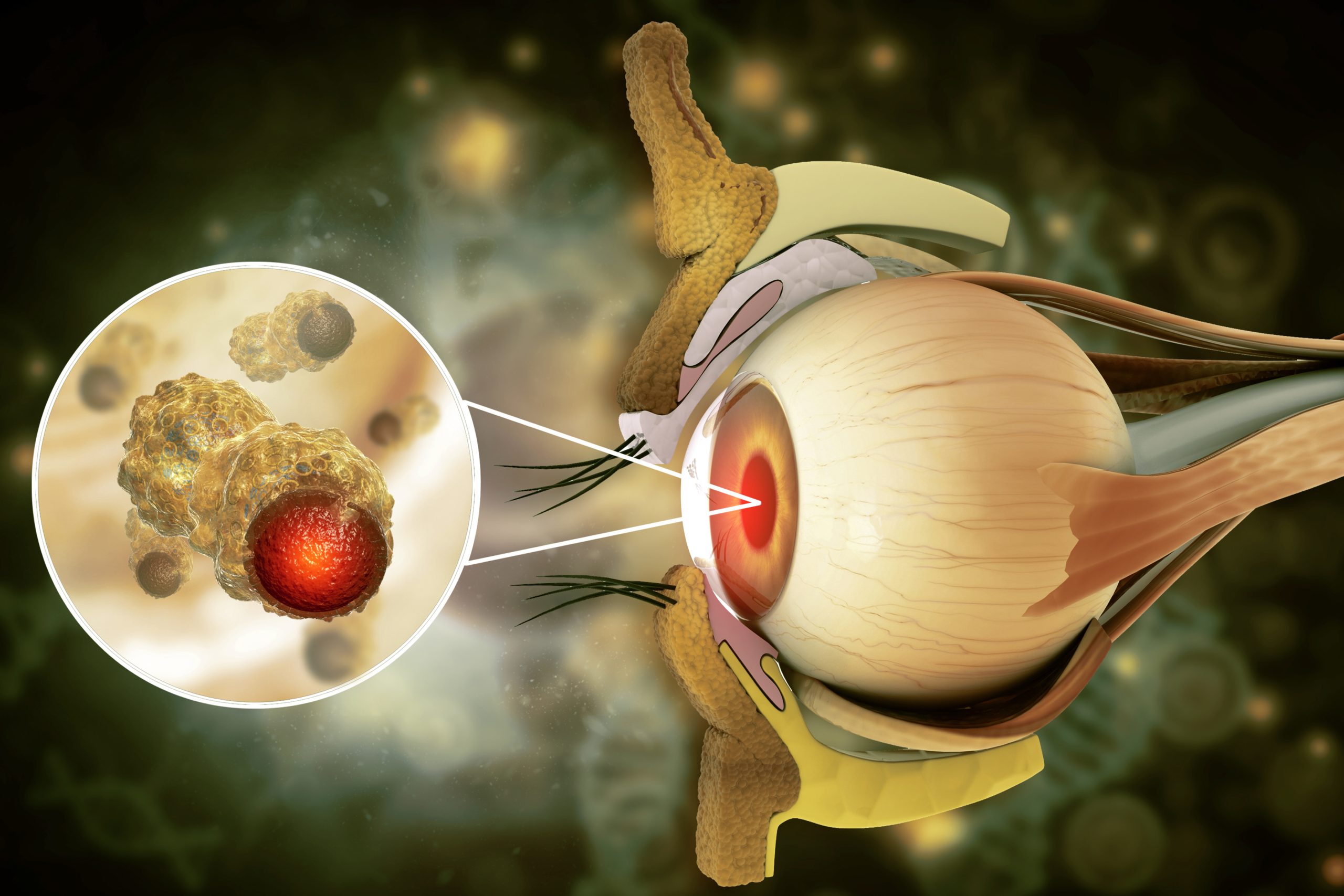
Biomechanics research contributes to the development of innovative diagnostic tools and therapeutic interventions for eye movement disorders. High-resolution imaging techniques, such as optical coherence tomography (OCT) and magnetic resonance imaging (MRI), enable detailed visualization of ocular structures and abnormalities associated with certain disorders.
Computational models of ocular biomechanics allow researchers to simulate various pathological conditions and test the efficacy of potential treatments, such as surgical interventions or rehabilitation protocols. By integrating biomechanical principles into clinical practice, healthcare professionals can offer personalized treatment plans tailored to each patient’s biomechanical profile and functional needs.
Biomechanical Analysis Techniques
- Motion Capture Systems: Explain how motion capture systems, such as infrared cameras and reflective markers, track the movement of ocular structures in three-dimensional space, providing precise data on eye movements.
- Electromyography (EMG): Detail how EMG recordings help identify muscle activation patterns during different types of eye movements, shedding light on neuromuscular control mechanisms.
- Finite Element Analysis (FEA): Discuss the application of FEA in modeling the mechanical behavior of ocular tissues under various loading conditions, offering insights into tissue deformation and stress distribution.
- Biomechanical Modeling: Explore computational models that simulate ocular biomechanics, including the role of muscle forces, tendon elasticity, and joint mechanics in generating and controlling eye movements.
Biomechanical Characteristics of Specific Disorders
- Strabismus Biomechanics: Investigate the biomechanical factors contributing to ocular misalignment in strabismus, such as muscle imbalance, contracture, or mechanical limitations within the eye socket.
- Nystagmus Mechanisms: Examine the biomechanical origins of involuntary eye movements in nystagmus, including abnormalities in the vestibulo-ocular reflex (VOR), neural feedback loops, and central nervous system dysfunction.
- Oculomotor Apraxia Biomechanics: Explore the biomechanical challenges associated with impaired voluntary eye movements in oculomotor apraxia, such as deficits in neural signal transmission, motor planning, or execution pathways.
Clinical Applications and Translational Research
- Diagnostic Biomarkers: Discuss emerging biomarkers derived from biomechanical analyses, such as ocular muscle stiffness, tendon tension, or neural conduction velocity, which may aid in early detection and monitoring of eye movement disorders.
- Personalized Treatment Approaches: Highlight how biomechanical insights inform personalized treatment strategies, such as customized surgical plans based on individual biomechanical profiles or tailored rehabilitation protocols targeting specific deficits.
- Technology Integration: Explore the integration of biomechanical data into advanced diagnostic tools, wearable devices, or virtual reality platforms for real-time assessment and training of ocular motor function.
Conclusion
Biomechanics research plays a vital role in deepening our understanding of eye movement disorders and guiding the development of novel diagnostic and therapeutic strategies. By leveraging biomechanical principles and advanced technology, researchers can unravel the complexities of ocular biomechanics and address the challenges posed by various eye movement disorders. Ultimately, this interdisciplinary approach holds the promise of improving clinical outcomes and enhancing the quality of life for individuals affected by these conditions.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Yes, several organizations and online communities provide support, information, and resources for individuals and families affected by eye movement disorders, offering guidance, advocacy, and peer support.
You can consult an ophthalmologist, neurologist, or optometrist with expertise in neuro-ophthalmology or pediatric ophthalmology, as they are trained to diagnose and manage various eye movement disorders.
Yes, factors such as excessive screen time, poor ergonomic habits, or inadequate rest can exacerbate symptoms of eye movement disorders by causing eye strain or fatigue.
Yes, targeted eye exercises or vision therapy programs may help enhance eye muscle strength, coordination, and control, leading to improvements in certain eye movement disorders.
Age-related changes in ocular muscles, nerves, or brain function can increase the risk of developing eye movement disorders, particularly conditions like age-related macular degeneration or presbyopia.
Yes, since eye movements are closely linked to balance and spatial orientation, certain eye movement disorders may impact overall coordination and stability.
Yes, some eye movement disorders are associated with underlying neurological conditions such as multiple sclerosis, Parkinson’s disease, or brainstem lesions.
Yes, trauma to the head or eye region can damage the nerves or muscles involved in controlling eye movements, leading to various types of eye movement disorders.
Yes, depending on the specific disorder, non-surgical treatments like vision therapy, prismatic lenses, or medication may be recommended to improve eye coordination and control.
Yes, certain eye movement disorders, such as congenital nystagmus or familial forms of strabismus, can have a genetic component, but the inheritance pattern can vary.
news via inbox
Subscribe here to get latest updates !