Hyphema: Navigating the Red Waters of Eye Injury
Embark on a journey to comprehend hyphema, a condition characterized by the accumulation of blood in the front chamber of the eye. This article acts as your guide, providing insights into the nature of hyphema, its causes, symptoms, and the importance of seeking immediate medical attention. Delve into risk factors, complications, diagnosis, treatment options, and practical measures for managing hyphema and promoting eye health.
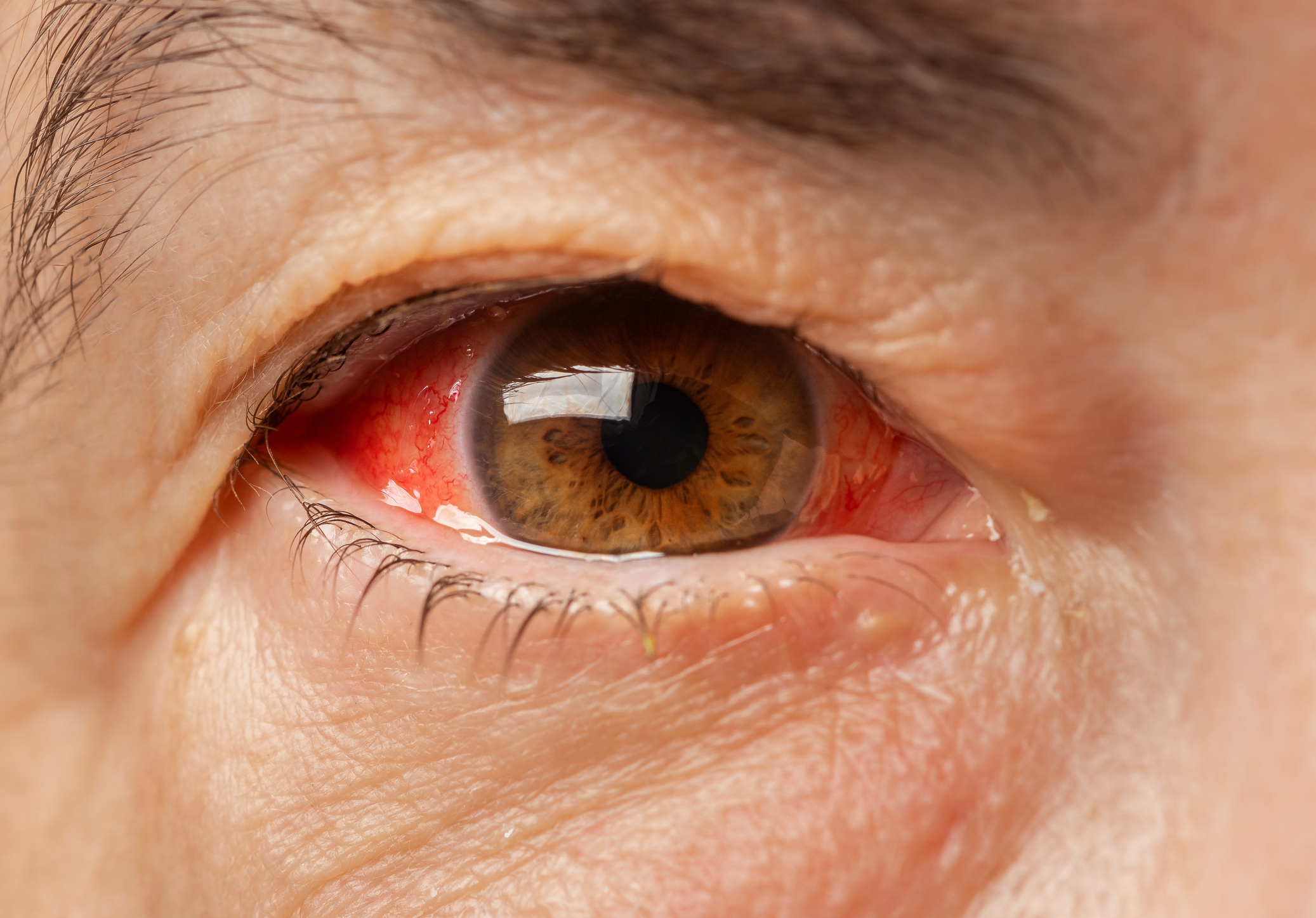
Overview of Hyphema
Hyphema is a condition characterized by bleeding within the anterior chamber of the eye, which is the space between the cornea (clear front part of the eye) and the iris (colored part of the eye). The presence of blood in this space can cause a visible layer of blood within the eye, affecting vision and potentially leading to complications.
Symptoms
- Visible Blood in the Eye: A visible layer or pool of blood in the front part of the eye is the primary symptom of hyphema.
- Eye Pain: Individuals with hyphema may experience eye pain or discomfort.
- Blurred Vision: The presence of blood can lead to blurred or obstructed vision.
- Increased Sensitivity to Light: Photophobia, or heightened sensitivity to light, may occur.
- Redness: The eye may appear red or have a reddish tint due to the presence of blood.
Causes
- Eye Trauma: Hyphema often results from trauma to the eye, such as a direct blow or injury.
- Eye Surgery: In some cases, hyphema can occur as a complication of eye surgery.
- Certain Medical Conditions: Underlying medical conditions, such as sickle cell disease, hemophilia, or blood clotting disorders, may increase the risk of hyphema.
- Certain Medications: Anticoagulant medications (blood thinners) or antiplatelet medications may contribute to bleeding in the eye.
- Eye Infections: Severe eye infections can lead to inflammation and bleeding in the anterior chamber.
What Happens Because of the Condition
The presence of blood in the anterior chamber can lead to several potential complications, including:
- Increased Intraocular Pressure: Hyphema can cause a rise in intraocular pressure, which may need to be closely monitored to prevent further damage.
- Secondary Glaucoma: Elevated intraocular pressure can potentially lead to secondary glaucoma, a condition that can cause optic nerve damage and vision loss.
- Corneal Blood Staining: Prolonged presence of blood in the anterior chamber can lead to corneal blood staining, affecting corneal clarity and visual function.
Risk Factors
- Eye Trauma: The most common risk factor is direct trauma to the eye, such as being hit by a projectile or experiencing a blunt force injury.
- Blood Disorders: Individuals with blood clotting disorders or conditions that affect blood vessel integrity may be at an increased risk.
- Anticoagulant Medications: Use of anticoagulant medications or antiplatelet drugs can increase the likelihood of bleeding in the eye.
- Age and Gender: Males and individuals in younger age groups are generally more susceptible to eye injuries and, consequently, hyphema.
Diagnosis
- Clinical Examination: Diagnosis is primarily based on a thorough clinical examination by an eye care professional.
- Visual Acuity Test: Testing the clarity of vision helps assess the impact of hyphema on visual function.
- Slit Lamp Examination: A slit lamp is often used to examine the anterior chamber and detect the presence and extent of blood.
- Intraocular Pressure Measurement: Monitoring intraocular pressure is crucial to assess the risk of complications such as glaucoma.
- Blood Tests: In cases where an underlying blood disorder is suspected, blood tests may be performed.
Treatment Options
- Rest and Head Elevation: Individuals with hyphema may be advised to rest and keep the head elevated to reduce intraocular pressure.
- Eye Shield: Wearing an eye shield can protect the eye from further trauma.
- Cycloplegic Medications: These medications help dilate the pupil and reduce the risk of complications.
- Pain Management: Pain relief medications may be prescribed to alleviate discomfort.
- Control of Intraocular Pressure: Medications or procedures may be recommended to control intraocular pressure and prevent glaucoma.
- Observation and Follow-up: Close monitoring of the condition is essential, and follow-up appointments may be scheduled to assess progress and address any changes.
Complications
- Increased Intraocular Pressure (IOP): Hyphema can lead to increased IOP, which, if left uncontrolled, may result in damage to the optic nerve and lead to glaucoma.
- Corneal Blood Staining: Prolonged presence of blood in the anterior chamber may cause corneal blood staining, impacting corneal clarity and visual function.
- Recurrent Bleeding: In some cases, there may be a risk of recurrent bleeding, especially if underlying conditions or risk factors are not addressed.
- Secondary Glaucoma: Persistent elevation of IOP can lead to secondary glaucoma, a serious condition that may cause irreversible vision loss if not managed promptly.
- Decreased Vision: Hyphema, if not properly managed, can result in decreased vision, particularly if complications such as glaucoma or corneal staining occur.
Prevention
- Protective Eyewear: Individuals engaged in activities with a risk of eye trauma, such as sports or certain occupations, should wear protective eyewear to reduce the likelihood of eye injuries.
- Safe Handling of Medications: If taking anticoagulant medications or blood thinners, it’s essential to follow the prescribed dosage and inform healthcare providers of any changes in medication.
- Avoidance of Risky Behaviors: Avoid engaging in activities that increase the risk of eye injuries, such as playing with sharp objects or engaging in activities without proper eye protection.
Medications
- Cycloplegic Agents: Cycloplegic medications, such as atropine or scopolamine, may be prescribed to dilate the pupil and reduce the risk of further bleeding.
- Pain Relief: Over-the-counter or prescription pain relief medications may be recommended to manage discomfort associated with hyphema.
- Topical Steroids: In certain cases, topical steroids may be prescribed to reduce inflammation.
- IOP-lowering Medications: If there is an elevation in intraocular pressure, medications such as beta-blockers or alpha agonists may be prescribed to manage IOP and prevent glaucoma.
When to See a Doctor
- After Eye Trauma: Seek immediate medical attention if there is a history of significant eye trauma, especially if there are symptoms like pain, blurred vision, or visible blood in the eye.
- Sudden Vision Changes: If there are sudden changes in vision, it’s crucial to see a doctor promptly.
- Persistent Eye Pain: Persistent or severe eye pain, especially after an injury, should be evaluated by a healthcare professional.
- Presence of Blood in the Eye: If there is visible blood in the eye, regardless of the cause, it warrants immediate medical attention.
Demographics More Susceptible
Individuals at a higher risk for hyphema include:
- Younger Age Groups: Children and young adults are more susceptible due to their engagement in activities with a higher risk of eye injuries.
- Males: Generally, males are more prone to eye injuries, making them more susceptible to hyphema.
- Certain Occupations and Activities: Individuals involved in activities or occupations with a higher risk of eye trauma, such as construction or sports, may be more vulnerable.
Follow-up Care for Adults and Children
- Adults: Follow-up care for adults with hyphema involves regular monitoring of intraocular pressure, visual function, and addressing any complications that may arise.
- Children: Pediatric patients with hyphema require specialized care, and follow-up appointments may include close monitoring of visual development, IOP, and any potential complications.
Conclusion
Hyphema is a serious eye condition that requires prompt medical attention to prevent complications and optimize outcomes. Whether caused by trauma or underlying medical conditions, early intervention, proper medications, and follow-up care are crucial elements of successful management. Protecting the eyes from potential injuries through preventive measures is also essential. With appropriate care and adherence to medical advice, individuals with hyphema can often achieve satisfactory recovery and minimize the risk of long-term complications.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
Wearing protective eyewear during sports activities can significantly reduce the risk of eye injuries and, consequently, the occurrence of hyphema.
Over-the-counter eye drops are not typically recommended for managing hyphema. Prescription medications, as prescribed by a healthcare professional, are more suitable.
While uncommon, hyphema can recur, especially if there is a risk of re-injury. Following medical advice and taking preventive measures are important.
In certain cases, bed rest and head elevation may be recommended to help minimize further bleeding and reduce intraocular pressure. Individualized medical advice is essential.
Hyphema may lead to increased intraocular pressure, which can contribute to the development of glaucoma. Monitoring and managing intraocular pressure are crucial.
Yes, hyphema can occur in individuals of all ages, including children. It is particularly important to seek immediate medical attention for pediatric cases.
In some cases, hyphema may occur without noticeable symptoms, especially in the early stages. However, visible blood in the eye is a clear sign of hyphema.
Surgery is not always required for hyphema. The treatment approach depends on the severity of the condition and the presence of complications.
Hyphema is typically associated with trauma or injury to the eye. Infections may cause other eye conditions but are not a common cause of hyphema.
With prompt and appropriate medical intervention, the majority of individuals with hyphema can recover without permanent vision loss. Timely treatment is crucial.
news via inbox
Subscribe here to get latest updates !