Living with Esotropia: Strategies for Coping and Treatment
Esotropia, commonly known as crossed eyes, is a condition where the eyes turn inward. This article provides a comprehensive overview of esotropia, covering its symptoms, causes, diagnosis, and treatment options for both children and adults. Learn when to see a doctor, the potential complications, risk factors, preventive measures, and how timely intervention can lead to successful management.
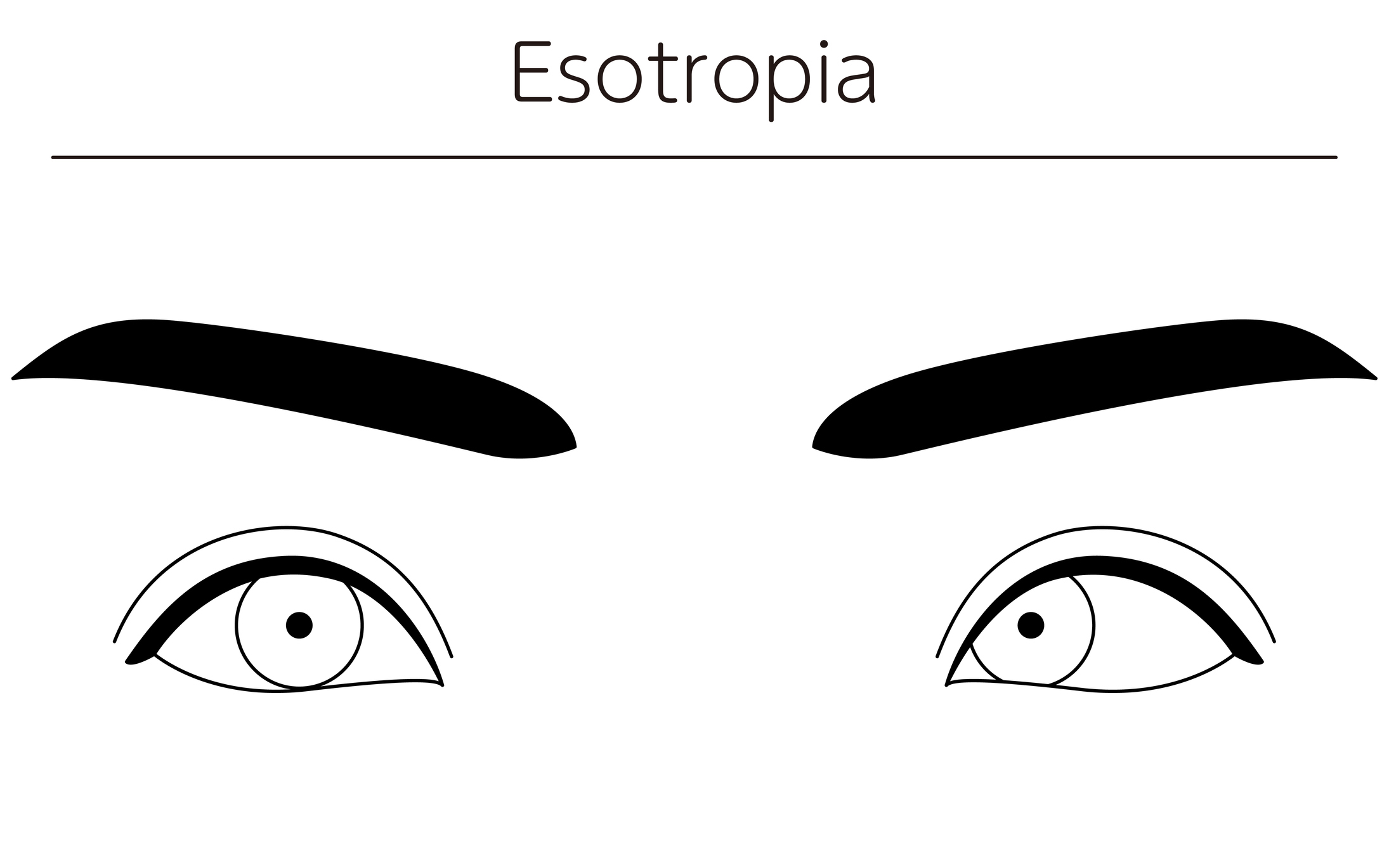
Overview of Esotropia
Esotropia, a form of strabismus, is a visual condition characterized by an inward deviation of one or both eyes. This ocular misalignment disrupts the parallel positioning of the eyes, leading to challenges in maintaining proper binocular vision. Understanding the intricacies of esotropia involves delving into its symptoms, underlying causes, and the effects it has on affected individuals.
Symptoms
The hallmark symptom of esotropia is the noticeable inward turning of one or both eyes. This misalignment may be constant or intermittent, depending on the specific subtype of esotropia. Individuals with esotropia may experience double vision (diplopia) due to the disparate positioning of the eyes, as the brain struggles to fuse conflicting visual inputs.
Other symptoms may include eye strain, fatigue, and difficulty focusing, especially when attempting to maintain a gaze on close-up objects. Children with esotropia may exhibit squinting, head tilting, or closing one eye to mitigate the effects of the misalignment.
Causes
Esotropia can stem from a variety of factors, both congenital and acquired. In congenital esotropia, the condition may be present from birth, often due to an imbalance in the extraocular muscles or a failure of the eyes to work together harmoniously. Acquired esotropia can develop later in life, triggered by factors such as refractive errors, muscle dysfunction, or neurological conditions.
Refractive errors, particularly hyperopia (farsightedness), are common contributors to esotropia. The eyes may overcompensate for the refractive error by inwardly turning to achieve clearer vision, leading to the characteristic misalignment.
What Happens Because of the Condition
The primary consequence of esotropia is compromised binocular vision, which can result in depth perception issues and visual discomfort. The brain may struggle to merge the images from each eye, leading to double vision and a reduced ability to accurately perceive the spatial relationships between objects.
In children, untreated esotropia can hinder visual development, potentially causing amblyopia (lazy eye). The brain may begin to favor one eye over the other, leading to reduced visual acuity in the less dominant eye.
Risk Factors
Several factors may heighten the risk of developing esotropia. Family history plays a significant role, as individuals with a family predisposition to strabismus or refractive errors may be more susceptible. Premature birth and low birth weight are additional risk factors, as these conditions may impact the proper development of the eye muscles and visual system.
Understanding these risk factors enables healthcare professionals to identify individuals who may benefit from early vision assessments, facilitating prompt intervention and minimizing the potential impact of esotropia on visual development.
Diagnosis
Diagnosing esotropia involves a comprehensive eye examination conducted by an eye care professional, often an optometrist or ophthalmologist. The diagnostic process includes a thorough assessment of visual acuity, eye alignment, and eye movement coordination. Specialized tests, such as the cover-uncover test and the alternate cover test, are employed to detect the presence and extent of ocular misalignment.
Refraction testing is crucial to identify any underlying refractive errors contributing to esotropia. Additionally, the examination may involve assessing the health of the eye structures and evaluating the extraocular muscles’ function.
Early diagnosis is essential, particularly in children, to prevent complications such as amblyopia. Regular eye screenings for infants and young children, coupled with prompt professional evaluation if any signs of strabismus are observed, contribute to timely intervention and optimal visual outcomes.
Treatment Options
The management of esotropia encompasses a variety of treatment modalities tailored to the specific needs and underlying causes of the condition.
- Glasses and Contact Lenses: Addressing refractive errors through the prescription of corrective lenses, such as glasses or contact lenses, is a common first-line intervention. Correcting hyperopia or other refractive errors can help align the eyes and reduce strain.
- Prism Lenses: Prism lenses may be prescribed to modify the light entering the eyes, aiding in the correction of ocular misalignment. Prisms can be incorporated into glasses to facilitate binocular vision and alleviate double vision.
- Vision Therapy: Vision therapy involves a structured program of eye exercises and activities designed to improve eye coordination and strengthen the eye muscles. It is often employed, especially in cases where muscle imbalances contribute to esotropia.
- Botulinum Toxin Injections: In certain cases, botulinum toxin injections may be considered to weaken specific eye muscles temporarily. This can be an option for those who do not respond well to other interventions or as a prelude to surgical procedures.
- Surgery: Strabismus surgery may be recommended to adjust the extraocular muscles’ length and alignment, restoring proper eye positioning. Surgical intervention is often considered when other non-invasive measures prove ineffective or in cases of persistent and significant misalignment.
The choice of treatment depends on factors such as the type of esotropia, its severity, and the individual’s overall eye health. A collaborative approach involving eye care professionals, parents, and patients is crucial in determining the most suitable treatment plan.
Complications
Untreated or inadequately managed esotropia can lead to various complications, with amblyopia being a significant concern. Amblyopia, or lazy eye, results from the brain favoring one eye over the other due to persistent ocular misalignment. Early intervention, including the correction of refractive errors and alignment issues, is vital to prevent amblyopia and promote optimal visual development.
Social and psychological complications may also arise, especially in cases where the visible misalignment becomes a source of self-consciousness or affects interpersonal relationships. Timely and effective treatment can address these challenges, fostering a positive impact on overall well-being.
Prevention
While certain risk factors for esotropia, such as family history, cannot be altered, there are preventive strategies that can contribute to maintaining ocular health:
- Regular Eye Check-ups: Routine eye examinations, starting in infancy and continuing throughout childhood and adulthood, facilitate the early detection and management of ocular issues, including esotropia.
- Prompt Intervention: Addressing refractive errors and strabismus promptly can mitigate the risk of complications, such as amblyopia. Early intervention is particularly crucial in children to optimize visual development.
- Eye Health Education: Promoting awareness of the importance of eye health, especially among parents and caregivers, can encourage proactive measures such as regular screenings and prompt professional evaluation if any signs of ocular misalignment are observed.
Medications
Medications play a limited role in the direct treatment of esotropia, primarily focusing on addressing underlying factors contributing to ocular misalignment. In cases where refractive errors, such as hyperopia, contribute to esotropia, prescription glasses or contact lenses are often the initial pharmaceutical intervention. These corrective lenses work to optimize vision and may help alleviate the strain on the eye muscles, promoting better alignment.
Additionally, for some individuals with accommodative esotropia, where excessive focusing effort leads to inward eye deviation, specific medications may be prescribed to relax the ciliary muscle and reduce the accommodative effort. However, medication alone is rarely the primary treatment for esotropia, and its use is typically integrated into a comprehensive management plan.
When to See a Doctor
Prompt consultation with an eye care professional is crucial if any signs or symptoms of esotropia are observed. These may include:
- Noticeable Eye Misalignment: If there is a consistent inward turning of one or both eyes.
- Double Vision: Experiencing double vision, especially when focusing on objects up close.
- Eye Strain or Fatigue: Persistent discomfort, strain, or fatigue while using the eyes, particularly during activities that require visual focus.
- Head Tilting or Squinting: Observing frequent head tilting or squinting, especially in children, to mitigate the effects of eye misalignment.
Early detection and intervention enhance the effectiveness of treatment and reduce the risk of complications, emphasizing the importance of seeking professional evaluation when any concerning signs emerge.
Demographics More Susceptible
Esotropia can affect individuals across various age groups, but certain demographics may be more susceptible. Children, particularly those with a family history of strabismus or refractive errors, are at an increased risk. Premature infants and those with low birth weight may also have a higher likelihood of developing esotropia, emphasizing the importance of regular eye examinations in these vulnerable populations.
While esotropia can manifest at any age, adults who experience sudden-onset or persistent eye misalignment should also seek prompt medical attention. Certain medical conditions or neurological changes in adulthood may contribute to the development of strabismus.
Follow-up Care for Adults and Children
Follow-up care is integral to monitor the progress of treatment and address evolving needs, particularly in children, whose visual systems are still developing. For children undergoing intervention, regular follow-up appointments with an eye care professional help assess treatment effectiveness, modify prescriptions as needed, and monitor ocular health.
Adults with esotropia, whether congenital or acquired, benefit from periodic check-ups to ensure that any changes in eye alignment or visual symptoms are promptly addressed. Follow-up care may include adjustments to corrective lenses, consideration of additional interventions if necessary, and ongoing monitoring for potential complications.
In children, follow-up care often extends to collaboration with educators and specialists to address any potential impact on learning and development. Early intervention services, if needed, can be incorporated into the follow-up care plan to support a child’s overall well-being.
Conclusion
In conclusion, esotropia presents a multifaceted challenge, requiring a tailored and comprehensive approach to management. Medications, when utilized, play a supportive role alongside other interventions such as corrective lenses, vision therapy, and, in some cases, surgical procedures. Early detection, timely intervention, and ongoing follow-up care are crucial components of effective esotropia management, ensuring optimal visual outcomes and overall eye health.
Whether in children or adults, collaboration between individuals, their families, and eye care professionals is vital in navigating the complexities of esotropia. As awareness grows and research advances, the hope is that improved understanding and personalized approaches to care will continue to enhance the quality of life for individuals affected by this ocular misalignment.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
In some cases, especially in children, Esotropia may improve or resolve with age. However, professional evaluation and appropriate treatment are essential for optimal outcomes.
Adults with Esotropia may experience sudden onset of double vision, especially if the eye misalignment becomes more pronounced. Immediate evaluation is recommended.
Esotropia can occur in individuals of any ethnic background. However, there may be some variations in prevalence among different populations.
Yes, Esotropia can be corrected without surgery in many cases. Non-surgical options, such as eyeglasses, patching, and vision therapy, are often effective, especially in children.
While Esotropia is often related to eye muscle imbalance, it can sometimes be associated with underlying health conditions. A comprehensive eye examination can help determine the cause.
Contact lenses can be an option for adults with Esotropia, but the choice between glasses and contact lenses depends on individual preferences and the eye care provider’s recommendations.
Esotropia itself does not typically lead to permanent vision loss. However, if left untreated, it can impact visual development, especially in children.
Prolonged screen time can contribute to eye strain, but it is not a direct cause of Esotropia. Regular breaks and proper vision correction can help alleviate eye strain.
No, surgery is one of several options. Eyeglasses, eye patching, vision therapy, and Botox injections are also common approaches, depending on the underlying cause.
Yes, Esotropia can develop in adults, but it is often diagnosed and treated in childhood. Adults experiencing eye misalignment should seek an eye examination.
news via inbox
Subscribe here to get latest updates !