Presumed Ocular Histoplasmosis Syndrome (POHS)
Presumed Ocular Histoplasmosis Syndrome (POHS) is an eye condition associated with a fungal infection. This article aims to provide clarity on the causes, symptoms, and practical approaches to managing POHS. Learn when to see a doctor, potential complications, risk factors, preventive measures, and the available treatments that contribute to improved eye health and overall well-being.
Overview of Presumed Ocular Histoplasmosis Syndrome
Presumed Ocular Histoplasmosis Syndrome (POHS) is an eye condition associated with exposure to the fungus Histoplasma capsulatum. While not everyone exposed to the fungus develops symptoms, those who do may experience a range of ocular issues. Let’s explore the various aspects of POHS.
Symptoms
POHS can manifest with various symptoms, including:
- Blurred Vision: Visual impairment or blurriness.
- Floaters: The perception of spots or specks moving in the field of vision.
- Scotomas: Dark or blank spots in the central vision.
- Distorted Vision: Straight lines appearing wavy or bent.
- Reduced Night Vision: Difficulty seeing clearly in low-light conditions.
These symptoms may affect one or both eyes and can vary in severity.
Causes
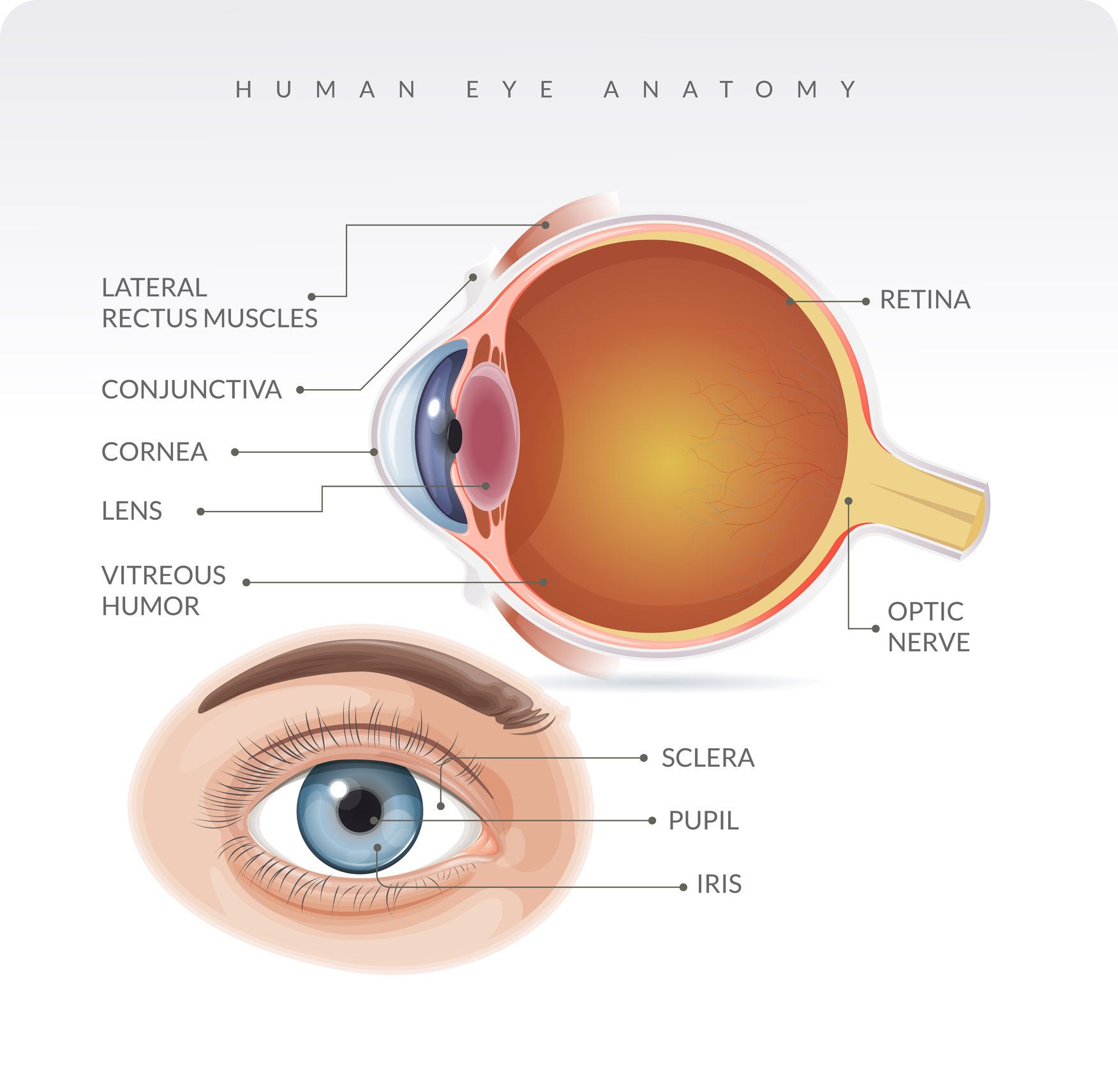
The primary cause of POHS is exposure to the fungus Histoplasma capsulatum. The fungus is commonly found in soil enriched with bird or bat droppings, and inhalation of airborne spores can lead to infection. POHS occurs when the infection affects the eyes, specifically the retina.
What Happens Because of the Condition
When Histoplasma capsulatum affects the retina, it can lead to:
- Chorioretinal Scars: Small, round scars on the retina, known as histo spots, which may or may not cause symptoms.
- Choroidal Neovascularization: Abnormal blood vessel growth beneath the retina, which can cause vision problems.
- Macular Edema: Swelling in the macula, the central part of the retina, leading to vision distortion.
Risk Factors
Certain factors may increase the risk of developing POHS:
- Geographic Location: Residing in or spending time in areas with a high prevalence of Histoplasma capsulatum, such as the Ohio and Mississippi River valleys in the United States.
- Exposure to Bird or Bat Droppings: Working in occupations or engaging in activities that involve exposure to environments with bird or bat droppings.
- Age: POHS is more common in individuals between the ages of 20 and 40.
Diagnosis
Diagnosing POHS involves a combination of clinical evaluation and imaging studies:
- Clinical Assessment: A comprehensive eye examination to assess visual acuity, examine the retina, and identify any symptoms.
- Fluorescein Angiography: Injecting a dye into the bloodstream to highlight blood vessels in the retina and identify abnormalities.
- Indocyanine Green Angiography: An imaging technique that provides additional information about the choroidal blood vessels.
- Optical Coherence Tomography (OCT): Producing detailed cross-sectional images of the retina to assess its thickness and identify any swelling.
- Visual Field Testing: Evaluating the field of vision to detect scotomas or abnormalities.
Early diagnosis is crucial for managing the condition and preventing complications.
Treatment Options
While there is no specific cure for Presumed Ocular Histoplasmosis Syndrome (POHS), treatment options focus on addressing complications and managing symptoms to preserve vision:
- Observation: In cases where the condition is asymptomatic or mild, and there is no active leakage or abnormal blood vessel growth, a watchful waiting approach may be recommended.
- Anti-VEGF Therapy: Intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) medications may be used to manage choroidal neovascularization and reduce abnormal blood vessel growth.
- Corticosteroids: In some cases, corticosteroids may be prescribed to reduce inflammation and control macular edema.
- Laser Photocoagulation: Laser treatment may be considered to seal leaking blood vessels and manage choroidal neovascularization.
- Photodynamic Therapy (PDT): PDT involves using a light-activated medication to selectively target abnormal blood vessels and reduce leakage.
Complications
Complications associated with POHS may include:
- Vision Loss: Progressive damage to the retina and complications such as choroidal neovascularization can lead to permanent vision loss if not effectively managed.
- Macular Edema: Swelling in the macula can cause central vision distortion and impairment.
- Choroidal Neovascularization: Abnormal blood vessel growth beneath the retina can result in bleeding and further vision problems.
Prevention
While it’s challenging to prevent Histoplasma capsulatum exposure entirely, certain measures may reduce the risk:
- Protective Measures: Use protective eyewear and masks when engaging in activities that may involve exposure to environments with bird or bat droppings.
- Geographic Awareness: Be aware of regions with a higher prevalence of Histoplasma capsulatum, such as the Ohio and Mississippi River valleys.
Medications
Several medications may be employed to manage symptoms and complications:
- Anti-VEGF Medications: Intravitreal injections of drugs like ranibizumab or bevacizumab can inhibit abnormal blood vessel growth.
- Corticosteroids: Oral or intravitreal corticosteroids may be prescribed to reduce inflammation.
- Photodynamic Therapy (PDT) Medication: A light-activated medication used in conjunction with PDT to target abnormal blood vessels.
When to See a Doctor
It is important to consult with an eye care professional if you experience:
- Vision Changes: Blurred vision, floaters, scotomas, or other visual disturbances.
- Eye Pain: Persistent eye discomfort or pain.
- Progressive Symptoms: Worsening or progressive symptoms related to vision.
- Known Exposure: If you have been exposed to environments with bird or bat droppings, especially in regions with a high prevalence of Histoplasma capsulatum.
Demographics More Susceptible
Demographic factors that may increase susceptibility to POHS:
- Geographic Residence: Individuals residing or spending significant time in regions with a high prevalence of Histoplasma capsulatum.
- Occupational Exposure: Those engaged in occupations or activities involving exposure to environments with bird or bat droppings.
- Age Group: POHS is more commonly diagnosed in individuals between the ages of 20 and 40.
Follow-up Care for Adults and Children
Follow-up Care for Adults:
- Regular Ophthalmologic Visits: Scheduled visits to monitor retinal changes, vision, and the effectiveness of interventions.
- Imaging Studies: Periodic imaging studies, such as fluorescein angiography and optical coherence tomography (OCT), to assess the status of the retina.
- Visual Acuity Testing: Regular assessments of visual acuity to detect any changes.
Conclusion
In conclusion, POHS presents unique challenges related to fungal exposure and subsequent ocular complications. Management involves a collaborative effort between healthcare professionals to preserve vision and address complications promptly. Regular follow-up care, early intervention, and adherence to preventive measures contribute to optimizing the long-term health of individuals affected by Presumed Ocular Histoplasmosis Syndrome.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
No, POHS is not contagious. It is linked to exposure to the Histoplasma fungus in specific environments.
While there’s no specific diet for POHS, maintaining a healthy diet supports overall well-being.
Smoking may be a risk factor, as it can weaken the immune system. Quitting smoking is beneficial for overall health, including eye health.
It’s possible, and ongoing monitoring is essential, especially for individuals with a history of exposure.
Currently, there is no vaccine, so preventive measures, including avoiding high-risk environments, are crucial.
Yes, POHS can affect both eyes, and the impact on each eye may vary.
Yes, some individuals may have asymptomatic Histoplasma infection, making regular eye check-ups important for early POHS detection.
Not always. With prompt treatment, vision loss can be minimized, and many individuals maintain functional vision.
It’s less likely, but possible. Regular eye check-ups are crucial for early detection, especially if symptoms arise.
While there is no cure, early and appropriate treatment can manage symptoms and prevent complications.
news via inbox
Subscribe here to get latest updates !