Macular Serous Detachment: Symptoms and Treatment
Introduction
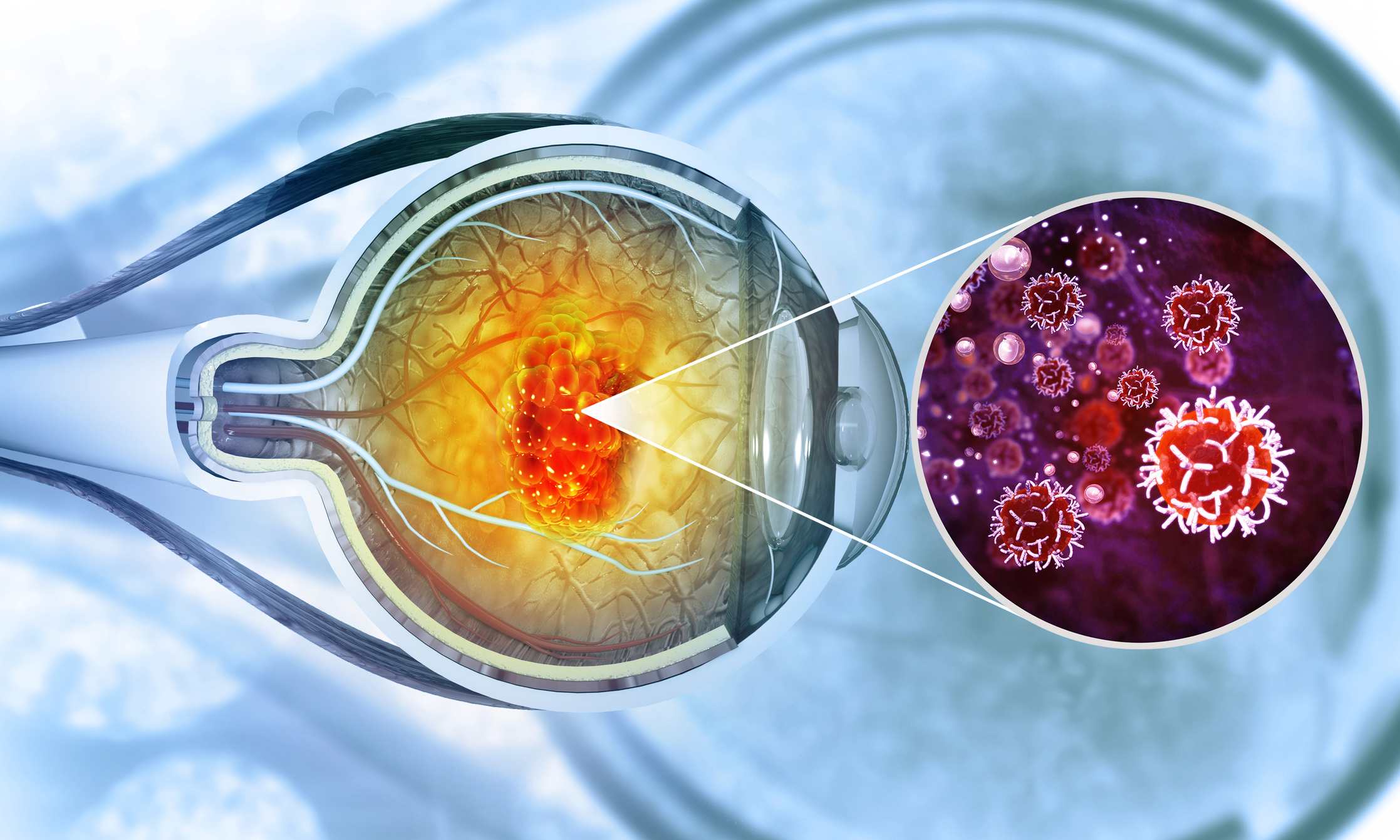
Macular serous detachment is a condition affecting the macula, the central part of the retina responsible for sharp, central vision. This condition occurs when fluid accumulates under the macula, leading to distortion and blurriness in central vision. In this article, we will explore the intricacies of macular serous detachment, including its causes, symptoms, and management options, to provide readers with a comprehensive understanding of this ocular condition.
What is Macular Serous Detachment?
Macular serous detachment, also known as central serous chorioretinopathy (CSC), is a disorder of the retina characterized by the accumulation of fluid beneath the macula. This buildup of fluid can lead to swelling and distortion of the macula, resulting in blurred or distorted central vision. While the exact cause of CSC is not fully understood, factors such as stress, corticosteroid use, and underlying medical conditions may contribute to its development.
Causes of Macular Serous Detachment
Several factors may contribute to the development of macular serous detachment, including:
- Stress: Emotional or physiological stress may trigger the release of stress hormones, which can affect the permeability of blood vessels in the retina, leading to fluid leakage.
- Corticosteroid use: Prolonged use of corticosteroid medications, whether oral, topical, or intravenous, has been associated with an increased risk of CSC.
- Hormonal changes: Certain hormonal imbalances, such as those occurring during pregnancy or with thyroid disorders, may predispose individuals to macular serous detachment.
- Genetics: There may be a genetic predisposition to CSC, with certain individuals being more susceptible to developing the condition.
- Systemic diseases: Conditions such as hypertension and autoimmune disorders have been linked to an increased risk of macular serous detachment.
Symptoms of Macular Serous Detachment
The symptoms of macular serous detachment may include:
- Blurred or distorted central vision.
- Reduced color perception.
- Metamorphopsia, or the perception of straight lines appearing wavy or bent.
- Central scotoma, or a blind spot in the center of vision.
- Micropsia, or objects appearing smaller than they are.
Management of Macular Serous Detachment
The management of macular serous detachment aims to reduce fluid accumulation, preserve vision, and prevent recurrence. Treatment options may include:
- Observation: In cases of mild CSC, where vision is not significantly affected, observation and regular monitoring may be recommended.
- Photodynamic therapy (PDT): PDT involves the use of a light-sensitive drug and laser treatment to target abnormal blood vessels and reduce fluid leakage.
- Anti-vascular endothelial growth factor (anti-VEGF) therapy: In some cases, injections of anti-VEGF medications may help reduce fluid accumulation and improve vision.
- Focal laser photocoagulation: Laser treatment can be used to seal leaking blood vessels and reduce fluid leakage in the macula.
- Corticosteroids: In certain situations, corticosteroid medications may be prescribed to reduce inflammation and fluid buildup in the retina.
Diagnosis of Macular Serous Detachment
Diagnosing macular serous detachment typically involves a comprehensive eye examination by an ophthalmologist or optometrist. The diagnostic process may include:
- Visual Acuity Testing: The doctor will assess your visual acuity using an eye chart to determine the clarity of your central and peripheral vision.
- Ophthalmoscopy: During this examination, the doctor will use a special instrument called an ophthalmoscope to examine the back of your eye, including the retina and macula. This allows them to identify any signs of fluid accumulation or other abnormalities.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging test that provides detailed cross-sectional images of the retina. It allows the doctor to visualize the thickness and structure of the macula, helping to confirm the presence of fluid accumulation and assess its severity.
- Fluorescein Angiography: In this test, a fluorescent dye is injected into a vein in your arm, and special photographs are taken as the dye circulates through the blood vessels in your eye. This helps to identify any leaking blood vessels or abnormalities in the retina.
- Fundus Autofluorescence (FAF): FAF imaging can provide additional information about the health of the retinal pigment epithelium (RPE), which plays a crucial role in maintaining the integrity of the retina.
When to Consult a Doctor
It is important to consult an eye care professional if you experience any symptoms suggestive of macular serous detachment, such as blurred or distorted central vision, changes in color perception, or visual disturbances. Additionally, if you have been diagnosed with macular serous detachment and experience any worsening of symptoms, new visual disturbances, or signs of complications, such as sudden vision loss or the appearance of floaters or flashes of light, you should seek prompt medical attention. Early diagnosis and appropriate management are crucial for optimizing visual outcomes and preventing long-term complications associated with macular serous detachment.
Conclusion
Macular serous detachment is a vision-threatening condition characterized by the accumulation of fluid beneath the macula. While the exact cause of CSC remains unclear, several factors may contribute to its development. Early diagnosis and appropriate management are crucial for preserving vision and preventing long-term complications. Individuals experiencing symptoms of macular serous detachment should seek prompt evaluation and treatment by an eye care professional to optimize visual outcomes and quality of life.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
In some cases, macular serous detachment can lead to permanent vision loss if left untreated or if there is significant damage to the macula.
While there may be a genetic predisposition to macular serous detachment, the condition is not always hereditary, and environmental factors also play a role in its development.
While stress has been linked to the development of macular serous detachment, more research is needed to determine the effectiveness of stress management techniques in preventing the condition.
Some studies suggest that a diet rich in antioxidants and omega-3 fatty acids may have protective effects on the retina and may help in managing macular serous detachment.
Yes, hormonal changes during pregnancy can increase the risk of macular serous detachment in some women. It is essential for pregnant individuals to monitor their vision and seek prompt medical attention if any changes occur.
Prolonged corticosteroid use, whether oral, topical, or intravenous, has been associated with an increased risk of macular serous detachment and may exacerbate the condition in some individuals.
While macular serous detachment can occur at any age, it is more commonly diagnosed in individuals between the ages of 30 and 50, with men being affected more frequently than women.
Laser eye surgery, such as LASIK or PRK, is not typically recommended for individuals with macular serous detachment, as it can potentially worsen the condition and lead to complications.
Lifestyle modifications such as quitting smoking, maintaining a healthy weight, and managing underlying health conditions like hypertension can help reduce the risk of recurrence of macular serous detachment.
Yes, macular serous detachment can be detected through a comprehensive eye examination, which may include visual acuity tests, dilated eye exams, and imaging tests such as optical coherence tomography (OCT).
news via inbox
Subscribe here to get latest updates !