Periorbital Cellulitis: Symptoms, Causes, and Treatment Strategies
Periorbital Cellulitis is a condition involving infection and inflammation around the eyes. This article aims to provide clarity on the causes, symptoms, and prompt eye care for Periorbital Cellulitis. Learn when to seek medical attention, potential complications, risk factors, preventive measures, diagnosis methods, treatment options, and insights for optimal eye health in individuals dealing with this condition.
Overview of Periorbital Cellulitis
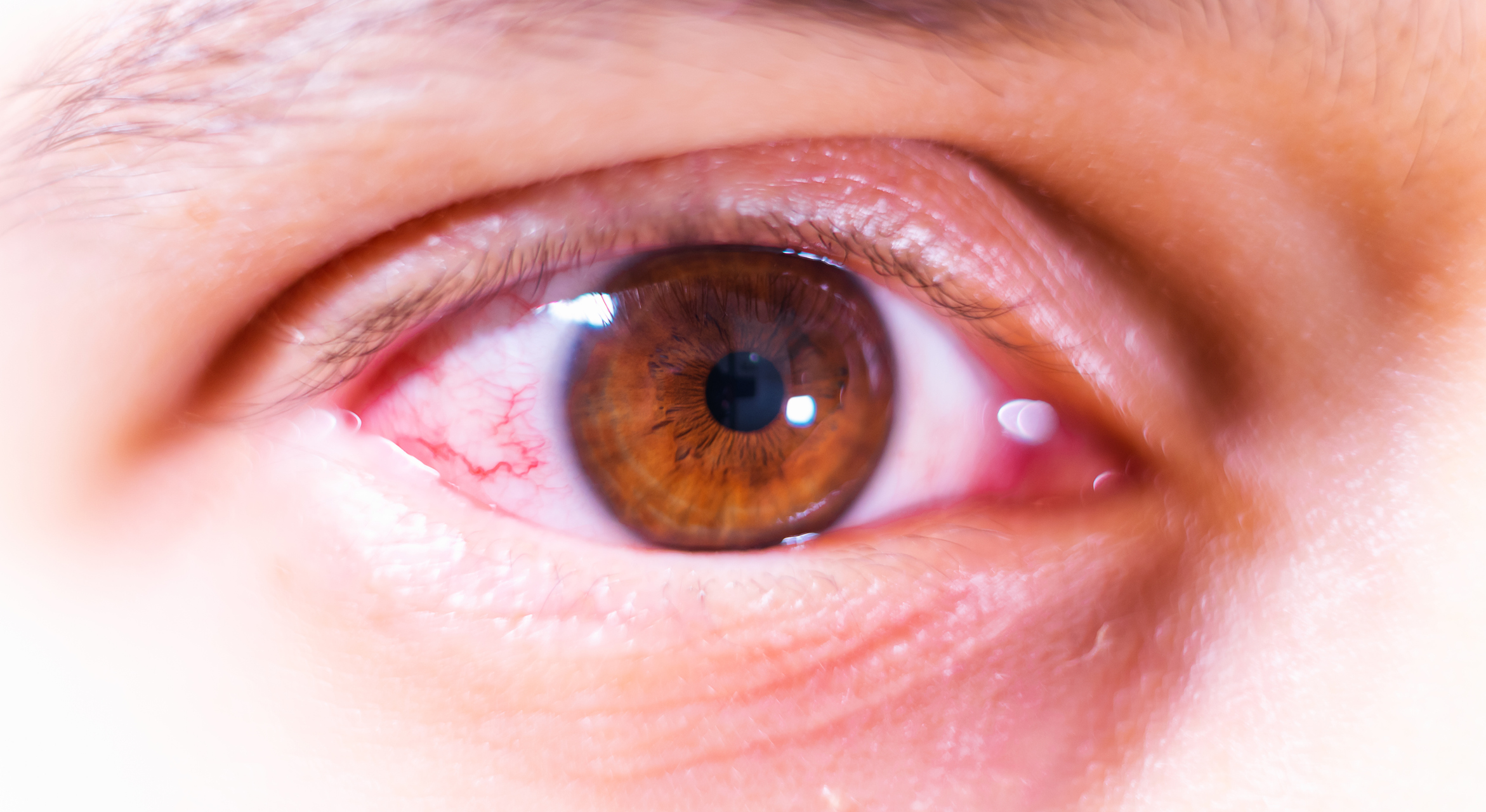
Periorbital cellulitis is a bacterial infection that affects the tissues surrounding the eye, specifically the eyelids and the skin around the eye socket (orbit). Unlike orbital cellulitis, which involves infection within the eye socket, periorbital cellulitis is limited to the outer tissues.
Symptoms
- Swelling: The affected area around the eye becomes swollen, often leading to a puffy appearance.
- Redness: The skin around the eye may appear red and inflamed.
- Pain or Tenderness: Pain or tenderness in the periorbital region, especially when touched.
- Warmth: The affected area may feel warm to the touch.
- Fever: In some cases, individuals may experience a fever.
- Discharge: Discharge from the eye, especially if the infection started with or involves a pre-existing eye condition.
Causes
- Bacterial Infection: Periorbital cellulitis is commonly caused by bacteria, with Staphylococcus aureus and Streptococcus species being common culprits.
- Entry Points: Bacteria can enter the periorbital tissues through breaks in the skin, insect bites, or as a complication of pre-existing eye infections.
What Happens Because of the Condition
- Inflammation of Tissues: Bacterial invasion leads to inflammation of the tissues surrounding the eye.
- Fluid Accumulation: Swelling occurs as a result of fluid accumulation in the affected area.
- Cellulitis Progression: Without prompt treatment, the infection can spread, leading to more severe complications.
Risk Factors
- Age: Children, especially those under the age of six, are more susceptible to periorbital cellulitis.
- Pre-existing Eye Conditions: Individuals with pre-existing eye conditions, such as conjunctivitis or a stye, may be at an increased risk.
- Upper Respiratory Infections: Respiratory infections, such as sinusitis, can serve as a source for bacterial spread to the periorbital region.
- Skin Trauma or Injury: Breaks in the skin, whether from trauma, insect bites, or other injuries, increase the risk of bacterial entry.
- Compromised Immune System: Individuals with a weakened immune system, due to conditions like diabetes or immunosuppressive medications, are at higher risk.
Diagnosis
- Clinical Examination: A healthcare professional will conduct a thorough examination of the affected eye and surrounding tissues, assessing for characteristic signs of periorbital cellulitis such as swelling, redness, and tenderness.
- Medical History: Gathering information about the patient’s medical history, recent illnesses, and any pre-existing eye conditions.
- Blood Tests: Blood tests, including a complete blood count (CBC), may be performed to assess for signs of infection and inflammation.
- Imaging Studies: In some cases, imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI) may be ordered to evaluate the extent of the infection and rule out orbital involvement.
Treatment Options
- Antibiotics: The primary treatment involves the administration of antibiotics to target and eliminate the causative bacteria. Oral antibiotics are often prescribed, but in severe cases, intravenous antibiotics may be necessary.
- Pain Management: Over-the-counter pain relievers may be recommended to alleviate pain and discomfort.
- Warm Compresses: Applying warm compresses to the affected area can help reduce swelling and promote drainage.
- Rest and Elevation: Resting and keeping the head elevated can aid in reducing fluid accumulation and promoting healing.
Complications
- Orbital Cellulitis: If left untreated or inadequately managed, periorbital cellulitis can progress to orbital cellulitis, a more severe infection involving the eye socket.
- Abscess Formation: In some cases, an abscess may form, requiring drainage.
- Spread of Infection: The infection can potentially spread to adjacent structures, leading to systemic complications.
Prevention
- Prompt Treatment of Eye Infections: Timely and appropriate treatment of pre-existing eye conditions, such as conjunctivitis or styes, can reduce the risk of secondary bacterial infections.
- Good Hygiene Practices: Practicing good hygiene, including proper handwashing, can help prevent the introduction of bacteria into the eyes.
- Avoiding Trauma: Taking precautions to avoid trauma to the eye, such as using protective eyewear during activities with a risk of injury.
Medications
- Antibiotics: Oral or intravenous antibiotics are prescribed to target the specific bacteria causing the infection. Common antibiotics include amoxicillin-clavulanate, cephalexin, or clindamycin.
- Pain Relievers: Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may be recommended to manage pain and reduce inflammation.
- Topical Antibiotic Ointments: In some cases, topical antibiotic ointments may be prescribed for application to the affected area.
When to See a Doctor
- Swelling and Redness: If there is sudden or significant swelling and redness around the eye, especially if it is accompanied by pain or tenderness.
- Eye Discharge: The presence of eye discharge, particularly if it is associated with increasing redness and swelling.
- Fever: If an individual experiences a fever along with symptoms of periorbital cellulitis, it is important to seek medical attention.
- Worsening Symptoms: If symptoms worsen despite home care measures or if there is no improvement within 24-48 hours.
- Vision Changes: Any changes in vision, such as blurred vision or difficulty seeing, should prompt immediate medical evaluation.
- Systemic Symptoms: The development of systemic symptoms such as nausea, vomiting, or lethargy may indicate a more severe infection.
Demographics More Susceptible
- Children: Children, especially those under the age of six, are more susceptible to periorbital cellulitis.
- Individuals with Pre-existing Eye Conditions: Those with pre-existing eye conditions, such as conjunctivitis or styes, may have an increased risk.
- Compromised Immune System: Individuals with a weakened immune system, due to conditions such as diabetes or immunosuppressive medications, may be more vulnerable.
Follow-up Care for Adults and Children
Follow-up Care for Children:
- Pediatric Ophthalmologist: A follow-up visit with a pediatric ophthalmologist may be recommended to assess the child’s eye health.
- Educational Support: Children who miss school days due to periorbital cellulitis may benefit from educational support services.
Follow-up Care for Adults:
- Ophthalmologist Visit: Adults should schedule a follow-up visit with an ophthalmologist or healthcare provider to monitor the progression of recovery.
- Systemic Health Check: Individuals with pre-existing health conditions, such as diabetes, should ensure regular follow-up appointments for overall health monitoring.
- Adjustment of Treatment Plan: Depending on the response to treatment, adjustments may be made to the antibiotic regimen or other management strategies.
Conclusion
In conclusion, prompt medical attention is crucial if an individual experiences symptoms of periorbital cellulitis, especially in high-risk groups such as children or those with compromised immune systems. Seeking medical care at the onset of symptoms and adhering to prescribed treatments are key to preventing complications and ensuring optimal recovery. Follow-up care is essential for both children and adults to monitor the resolution of symptoms and address any lingering concerns. While periorbital cellulitis can be a concerning condition, early intervention and appropriate follow-up care contribute to successful outcomes and the maintenance of good eye health.
World Eye Care Foundation’s eyecare.live brings you the latest information from various industry sources and experts in eye health and vision care. Please consult with your eye care provider for more general information and specific eye conditions. We do not provide any medical advice, suggestions or recommendations in any health conditions.
Commonly Asked Questions
In most cases, with timely and appropriate treatment, Periorbital Cellulitis does not lead to vision loss. However, severe cases and complications may require vigilant management.
While uncommon, a bug bite that breaks the skin can potentially lead to Periorbital Cellulitis. Prompt wound care and infection prevention are crucial.
No, Periorbital Cellulitis requires prescription antibiotics. It is essential to consult a healthcare professional for proper diagnosis and appropriate treatment.
Recurrence is uncommon with proper treatment. Addressing underlying risk factors, maintaining good hygiene, and seeking timely care reduce the likelihood of recurrence.
While it can affect individuals of any age, Periorbital Cellulitis is more common in children, especially those with skin injuries or upper respiratory infections.
Yes, sinus infections are among the risk factors for Periorbital Cellulitis. Prompt treatment of sinus infections reduces the likelihood of complications.
Yes, warm compresses can help alleviate swelling and discomfort associated with Periorbital Cellulitis. They can be used in addition to prescribed treatments.
While it can occur in one or both eyes, Periorbital Cellulitis may affect one eye initially. Prompt treatment helps prevent the spread to the other eye.
Periorbital Cellulitis itself is not typically contagious. It is usually caused by bacterial infection, and transmission occurs through breaks in the skin rather than person-to-person contact.
With prompt and appropriate treatment, Periorbital Cellulitis is generally reversible without permanent eye damage. Timely intervention is crucial to prevent complications.
news via inbox
Subscribe here to get latest updates !